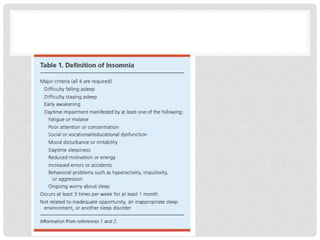
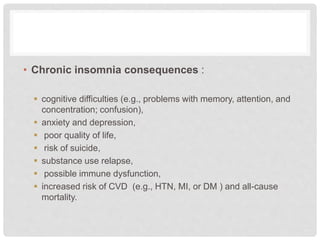
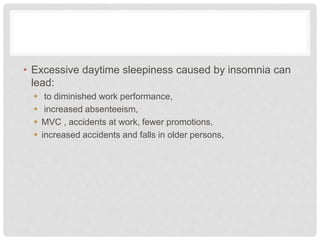
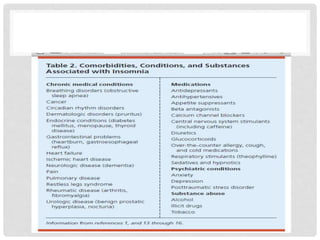
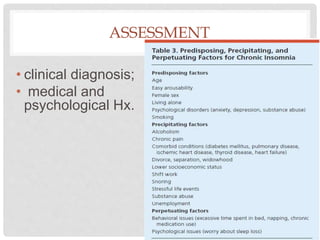
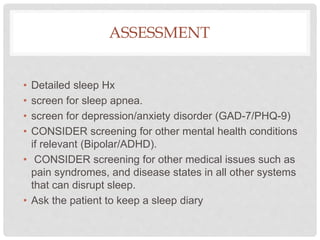
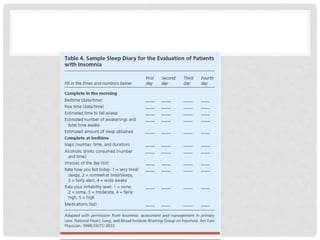
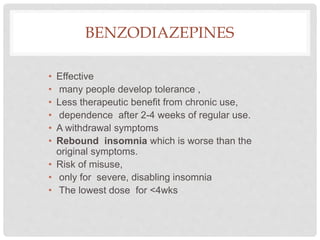
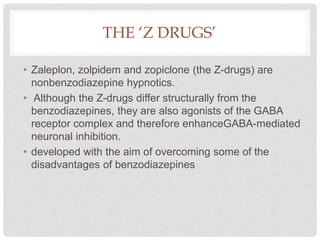
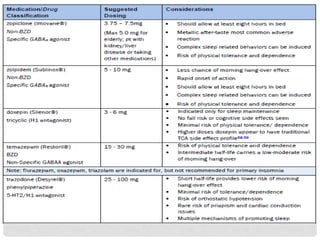
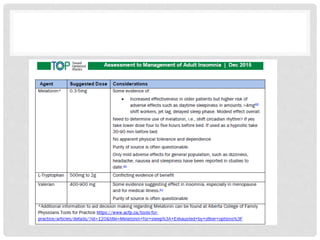
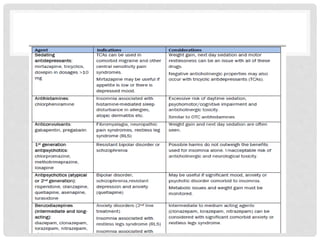
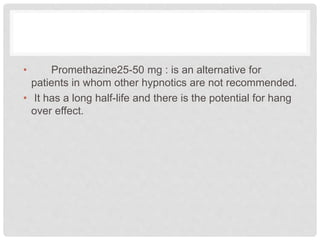
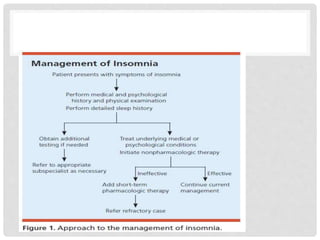
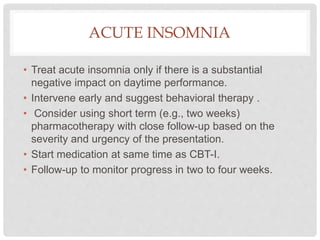
Insomnia is defined as difficulty falling asleep, staying asleep, or early awakening despite opportunities for sleep, associated with impaired daytime functioning for at least 3 nights per week for over a month. It can be acute (under 3 months) or chronic. Assessment involves evaluating sleep history, screening for sleep apnea and mental health issues. Treatment goals are improving sleep quality, decreasing distress, and improving daytime function. Non-pharmacological therapies like CBT, sleep hygiene, and sleep restriction are recommended initially. Hypnotics may be used short-term but have risks and should be avoided for chronic insomnia if possible. CBT-I is the cornerstone treatment and can be combined with short-term medication