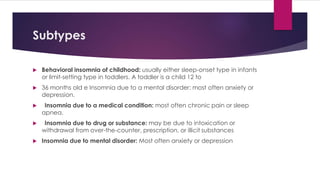
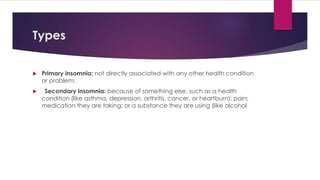
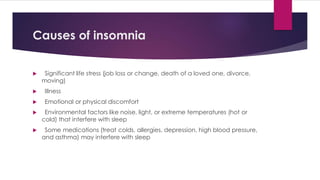
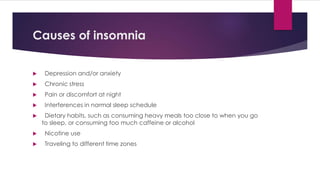
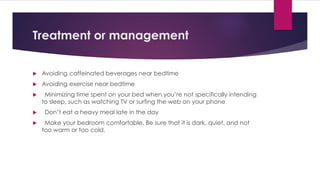
The document discusses insomnia, including its definition as difficulty falling or staying asleep, types such as chronic or short-term, common causes like stress or medications, symptoms like fatigue, and treatments including cognitive behavioral therapy, relaxation techniques, and sometimes prescription medications. Diagnosis involves keeping a sleep log and may include tests like a sleep study to evaluate nighttime sleep patterns.