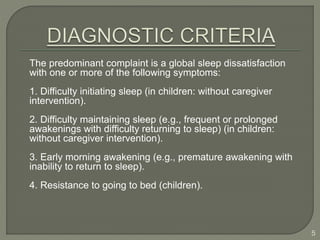
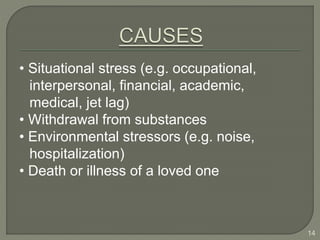
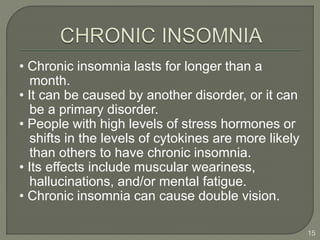
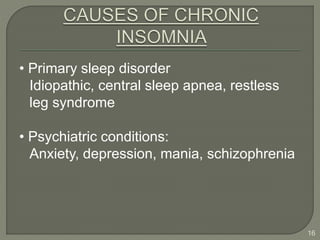
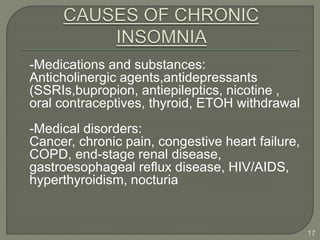
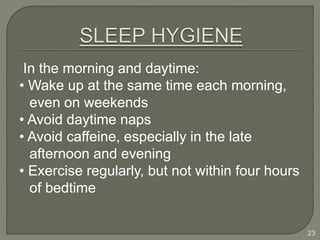
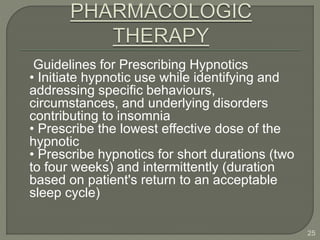
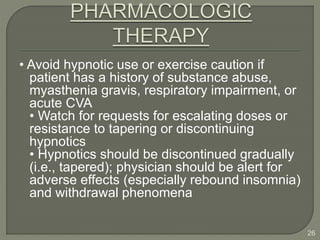
Insomnia is difficulty falling or staying asleep that interferes with daily life. It can be transient (less than a week), acute (less than a month), or chronic (over a month). Many factors can contribute to insomnia, including medical, psychiatric, and substance-related issues. Treatment involves both non-pharmacological options like cognitive behavioral therapy and relaxation techniques, as well as pharmacological options like benzodiazepines, but drugs should be used cautiously and for short durations. Proper sleep hygiene practices can also help manage insomnia symptoms.