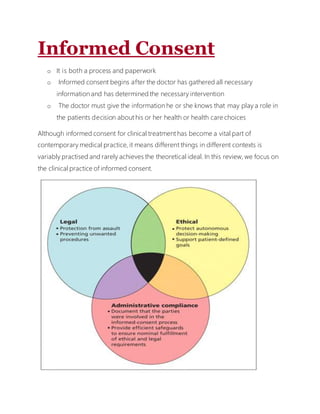
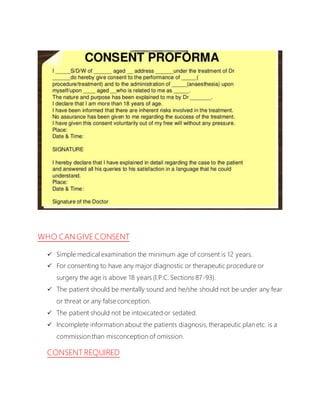
The document discusses the concept and practice of informed consent in clinical contexts. It covers informed consent from legal, ethical, and administrative perspectives. Legally, informed consent aims to protect patient autonomy and self-determination. Ethically, it seeks to make the medical decision-making process more patient-centered. Administratively, signed consent forms are used to document that a consent process occurred. The document also outlines common elements of informed consent discussions, including diagnosis, treatment options, risks/benefits, alternative treatments, and prognosis.