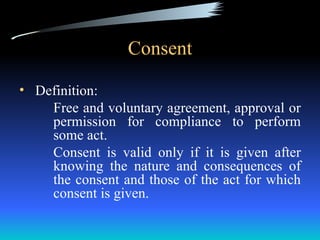
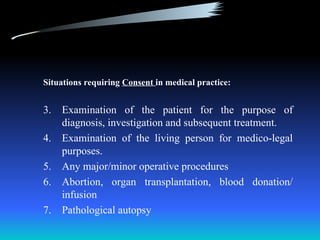
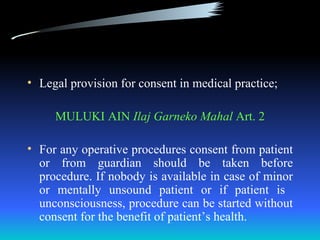
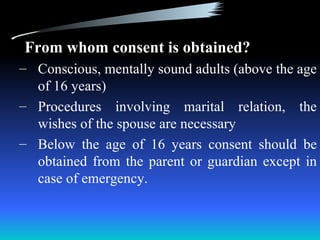
Consent involves obtaining free and voluntary approval from a patient for medical treatment or procedures, with key requirements being that the patient understands what they are consenting to and the potential consequences. There are different types of consent including implied, expressed, and informed consent, with informed consent being the standard that requires fully explaining treatment options and risks to ensure the patient can make an informed decision. Determining a patient's decision-making capacity is also important for valid consent.


![Informed Consent:
Standard And Disclosure
Q: How should the adequacy of
disclosure of information by a
physician be determined?
A: 3 approaches
[PHYSICIAN centered]
Ask what a reasonable and prudent
physician would tell a patient?](https://image.slidesharecdn.com/consentrs-120605092231-phpapp02/85/Consent-rs-20-320.jpg)
![[PATIENT centered]
What information would a reasonable
patient need to know to make an
rational decision?
[SUBJECTIVE or PATIENT SPECIFIC]
Whether the information provided is
specifically tailored to particular
patients need for information and
understanding](https://image.slidesharecdn.com/consentrs-120605092231-phpapp02/85/Consent-rs-21-320.jpg)
![ The trend is now going towards
[SUBJECTIVE or PATIENT SPECIFIC]
The reasonable - patient centered
standard may be ethically sufficient, but
the subjective standard is ethically ideal](https://image.slidesharecdn.com/consentrs-120605092231-phpapp02/85/Consent-rs-22-320.jpg)