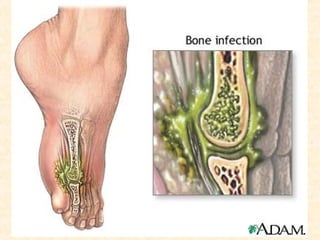
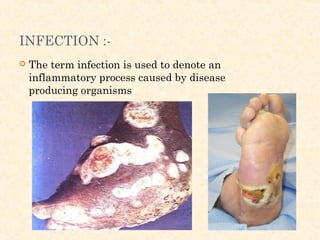
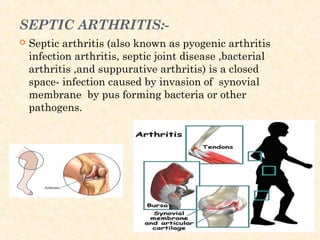
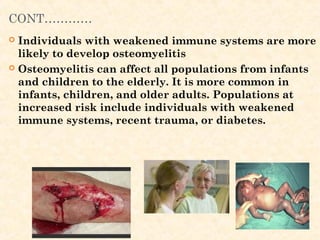
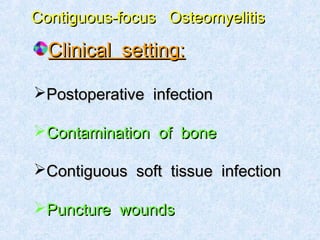
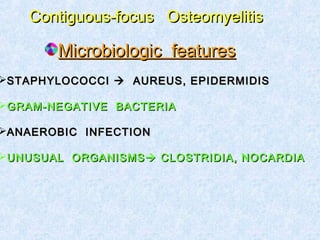
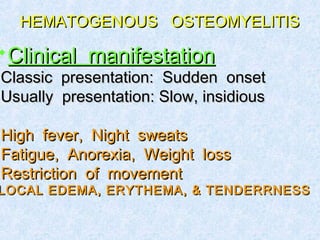
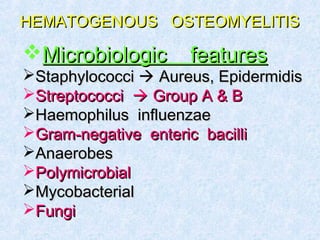
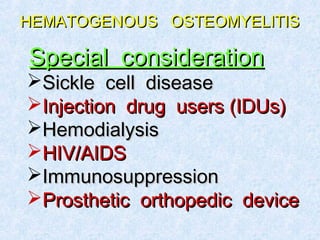
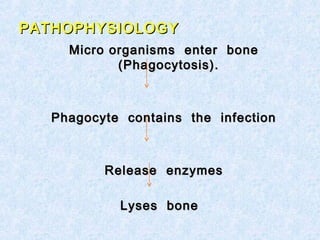
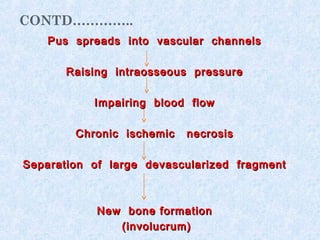
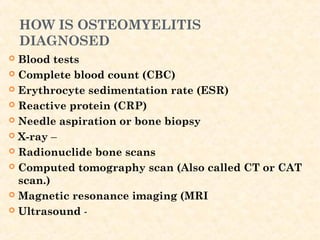
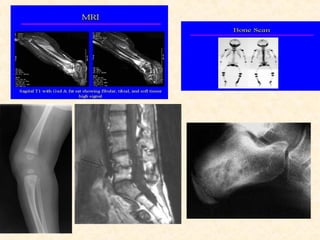
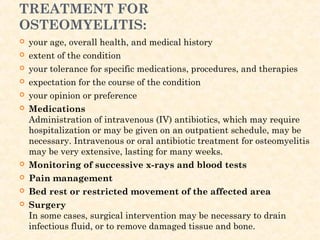
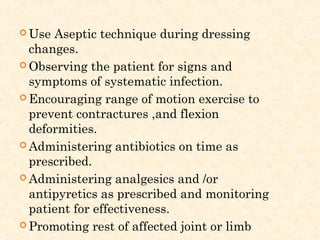
The document discusses bone infection or osteomyelitis, including causes such as bacterial infection spreading through the bloodstream or nearby tissue, symptoms like fever and bone pain, diagnosis through tests like blood work, x-rays and biopsies, and treatment involving long-term antibiotic therapy and sometimes surgery to drain infections and remove damaged tissue. Osteomyelitis can affect people of all ages but is more common in infants, children, and older adults.