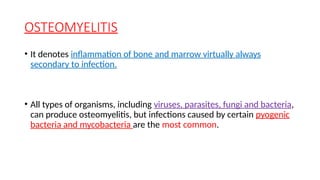
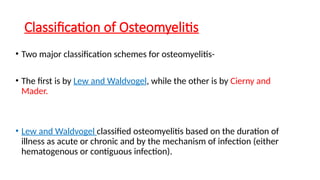
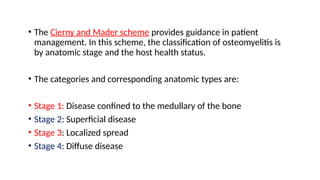
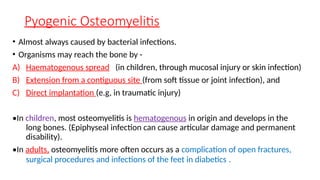
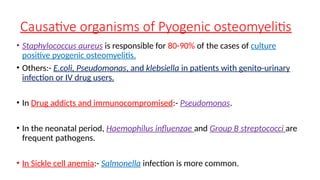
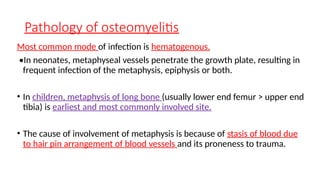
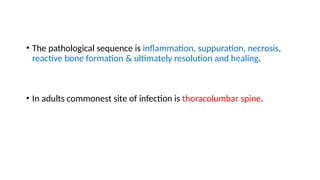
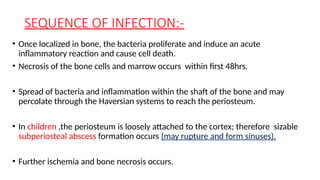
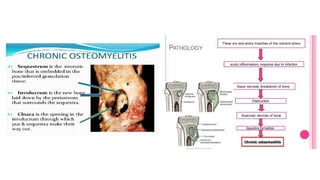
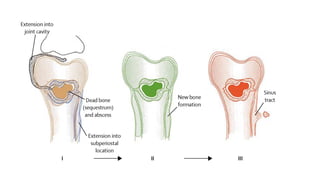
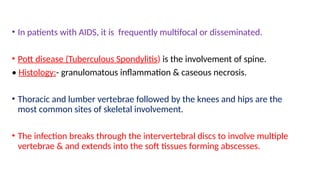
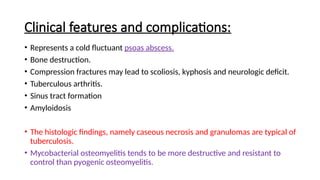
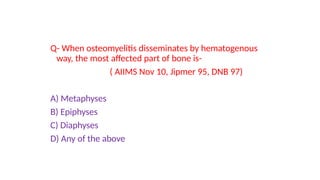
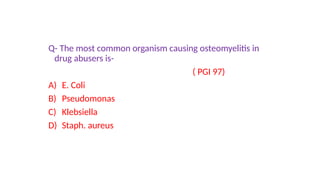
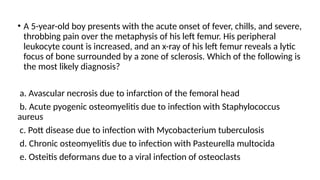
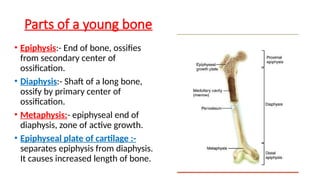
The document discusses the anatomy and functions of bones, detailing the composition of bone matrix and cellular components involved in bone formation and resorption. It focuses on osteomyelitis, including its classifications, pathology, and clinical features caused by pyogenic and tuberculous infections, as well as the common organisms involved. The document also outlines diagnostic methods and potential complications associated with osteomyelitis.
![Constituents of bone
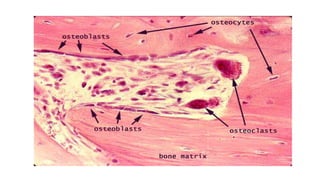
• An extracellular matrix and specialized cells responsible for production
and maintenance of the matrix.
• Bone matrix :- composed of an organic component known as osteoid
(35%) and a mineral component (65%).
• The unique feature of bone matrix, its hardness, is imparted by the
inorganic moiety hydroxyapatite [Ca10(PO4)6(OH)2 ], which also serves as a
repository for 99% of the body’s calcium and 85% of its phosphorus.
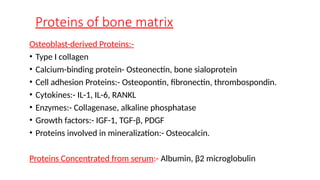
• Osteoid :- type I collagen + GAGs + other proteins](https://image.slidesharecdn.com/bone-1osteomyelitis-241204071346-66b2a91a/85/BONE-soft-tissue-Osteomyelitis-pathology-pptx-4-320.jpg)