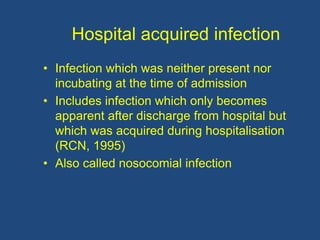
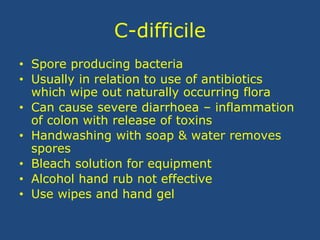
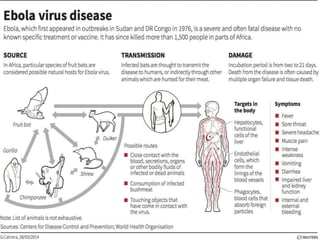
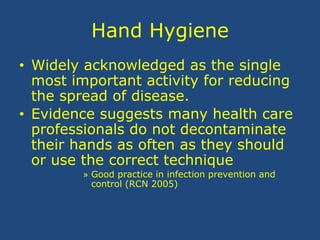
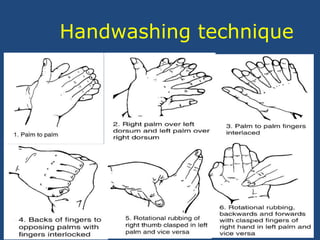
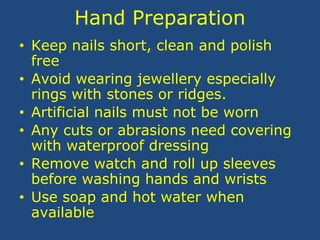
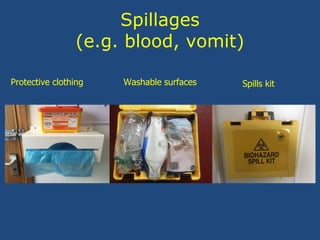
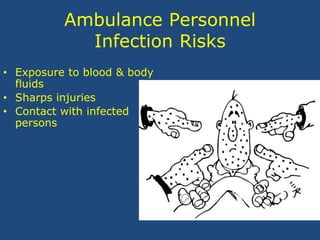
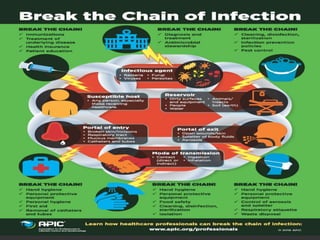
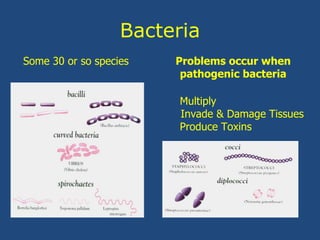
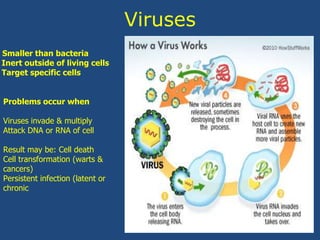
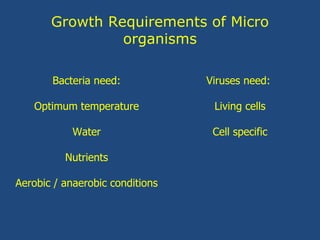
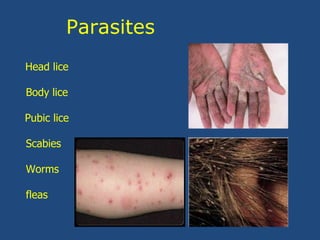
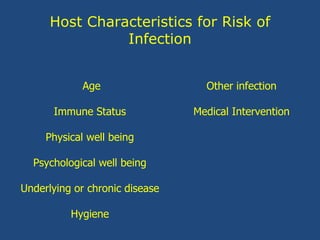
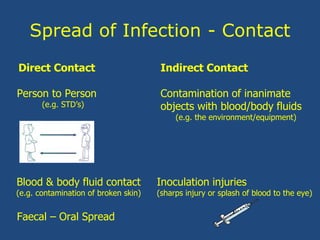
This document discusses infection control for ambulance personnel. It describes the chain of infection and how microorganisms like bacteria, viruses, and fungi can cause disease when they enter the body and reproduce. It also outlines the risks ambulance personnel face from exposure to blood, body fluids, and infected individuals. The document emphasizes the importance of universal precautions, hand hygiene, protective equipment, safe sharps handling, and cleaning and disposal of waste to prevent the spread of infection.

![The nature of infection
• Micro-organisms - bacteria, fungi, viruses,
protozoa and worms
• Most are harmless [non-pathogenic]
• Pathogenic organisms can cause infection
• Infection exists when pathogenic organisms
enter the body, reproduce and cause disease](https://image.slidesharecdn.com/infectioncontrol-171010203441/85/Infection-control-2-320.jpg)



![Healthcare acquired infection
• Incidence of 10%
• 5,000 deaths per year - direct result of HAI
• 15,000 deaths per year linked to HAI
• Delayed discharge from hospital
• Expensive to treat [£3,500 extra] per patient
• Cost to NHS - £1 billion per year
• Effective hand washing is the most effective
preventative measure
• Dirty environments and re-use of disposable
equipment also blamed
• Numbers are reducing](https://image.slidesharecdn.com/infectioncontrol-171010203441/85/Infection-control-16-320.jpg)