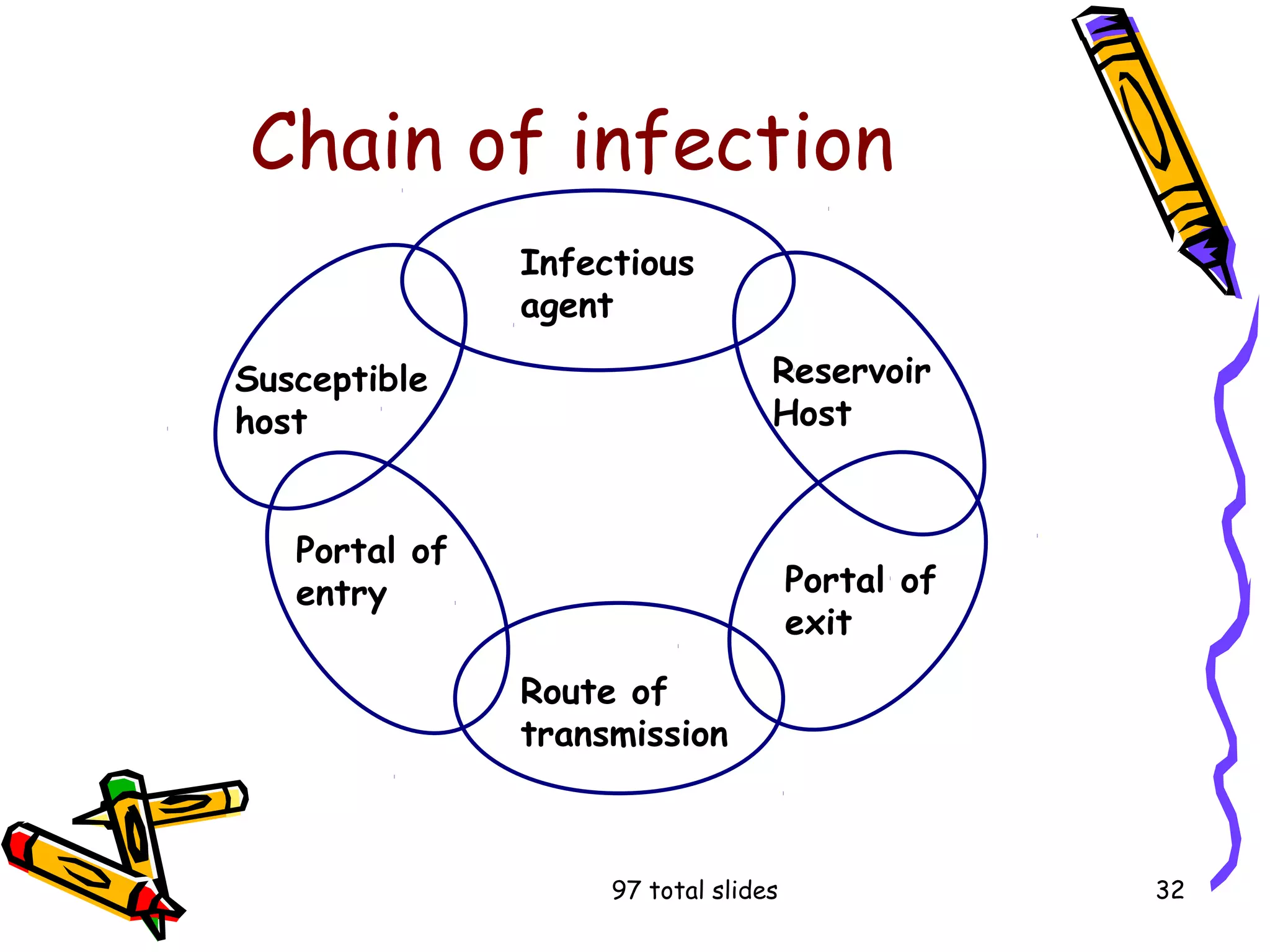
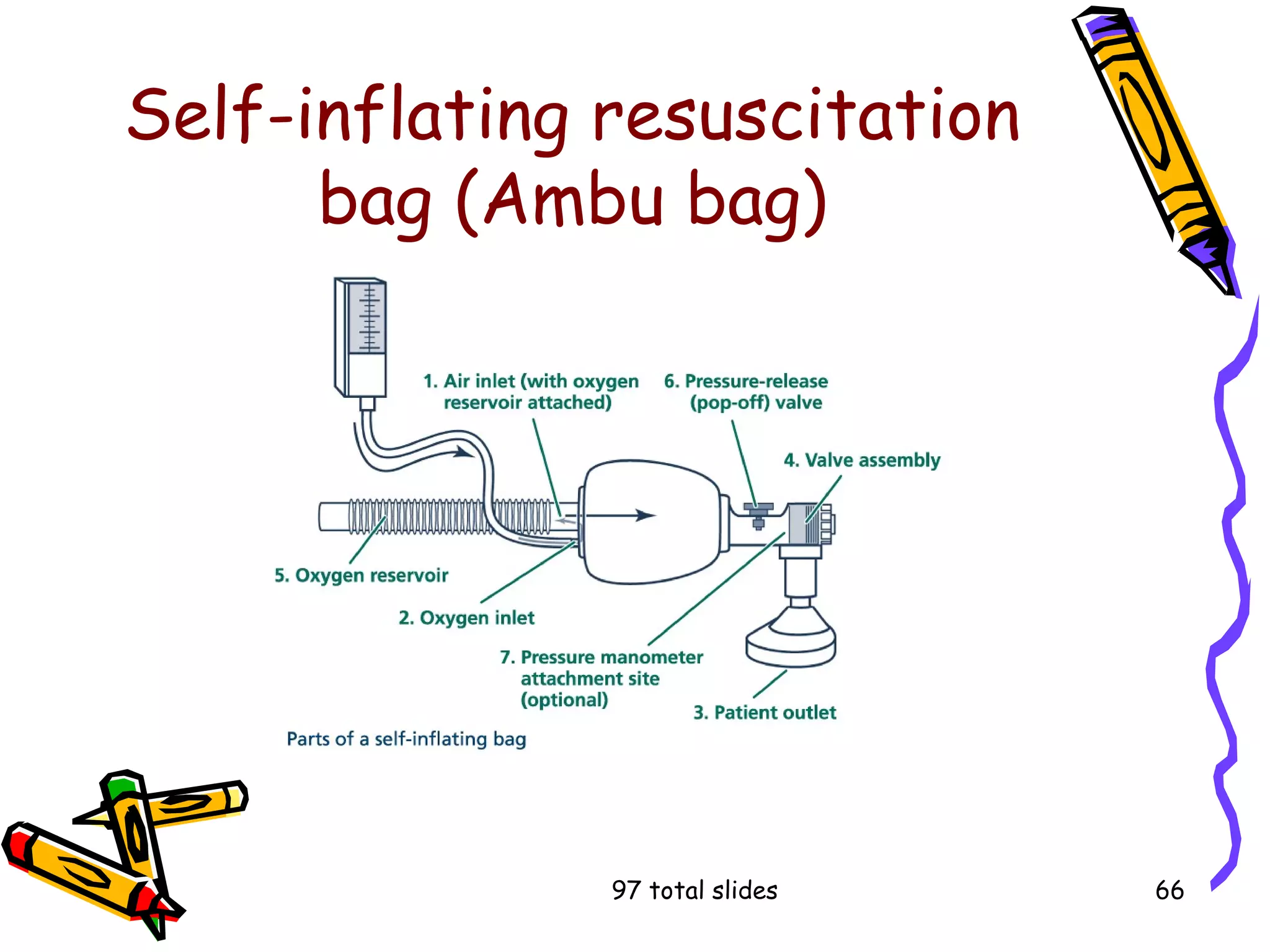
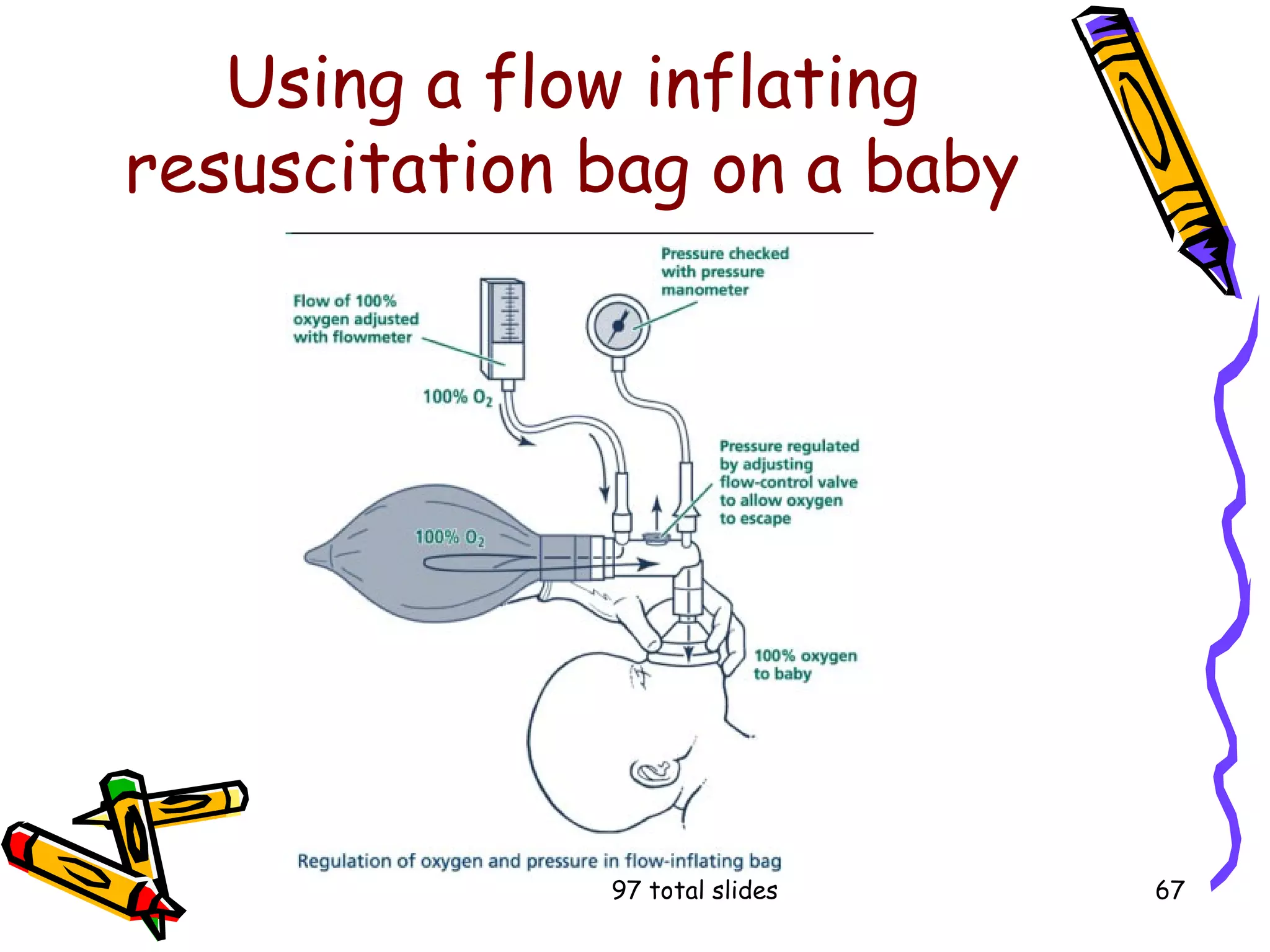
The document outlines the principles of infection prevention and control, emphasizing the importance of reducing the spread of infectious diseases caused by various pathogens. It details the chain of infection, types of microorganisms, their characteristics, and methods for preventing infections, including medical and surgical asepsis, proper hygiene, and the use of personal protective equipment. Additionally, it highlights the role of regulatory agencies like the CDC and OSHA in establishing guidelines to safeguard public health.