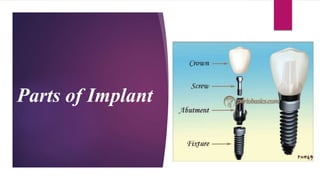
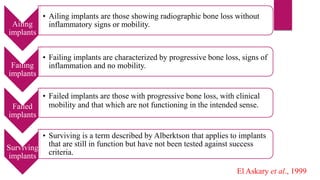
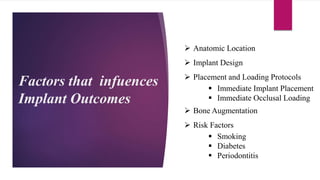
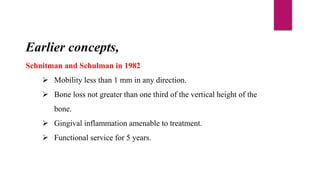
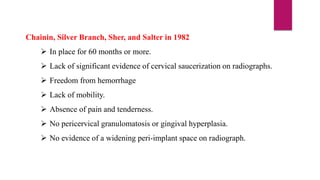
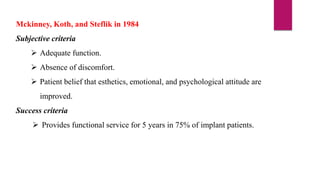
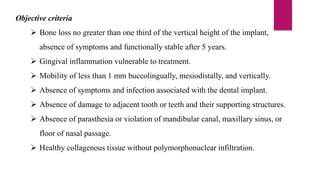
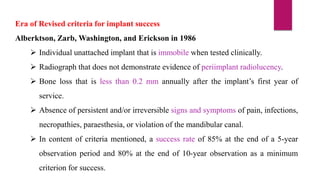
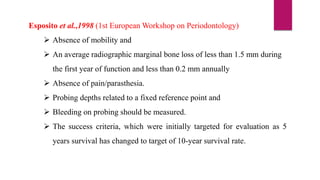
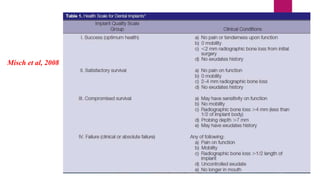
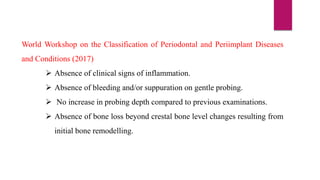
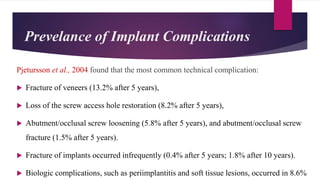
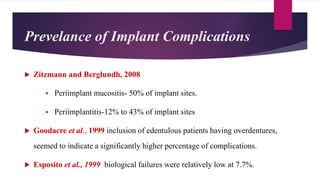
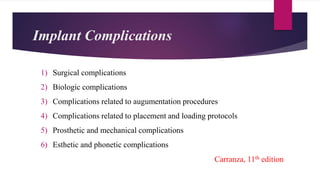
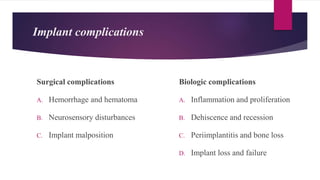
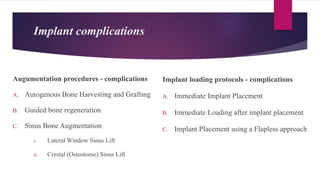
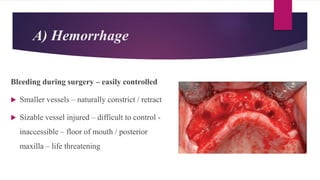
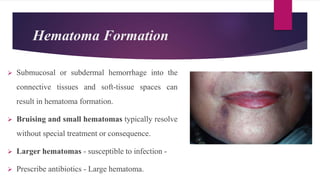
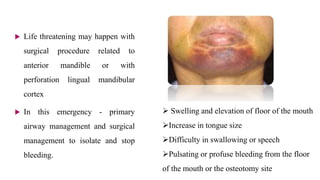
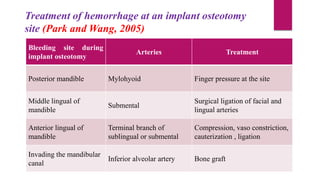
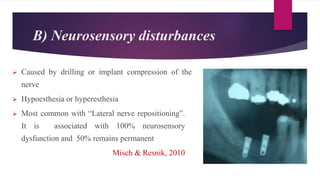
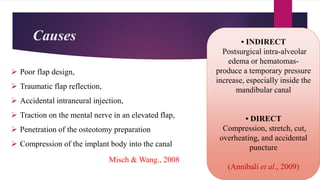
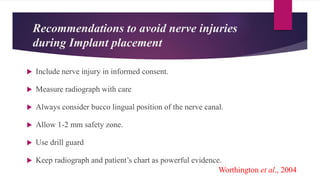
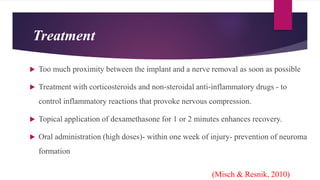
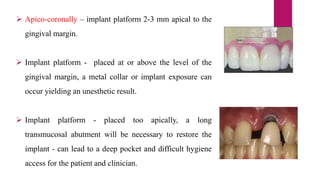
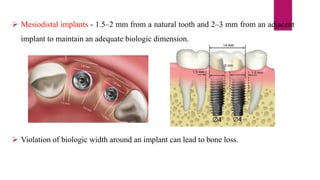
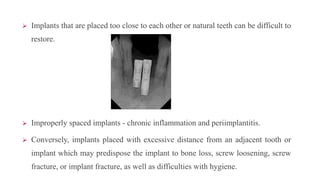
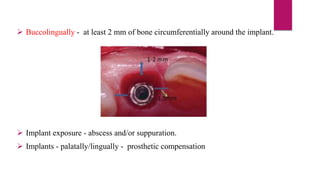
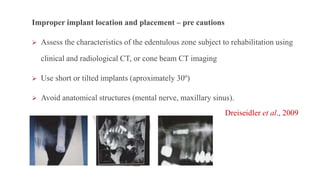
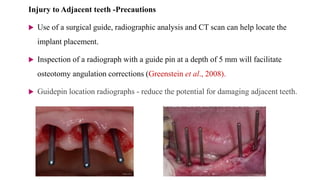
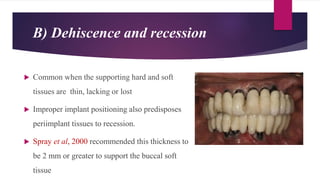
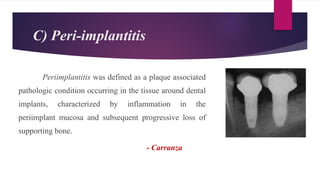
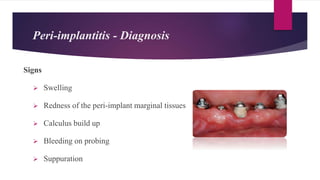
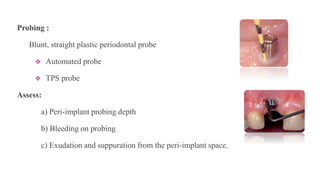
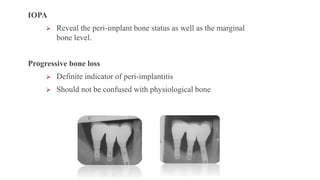
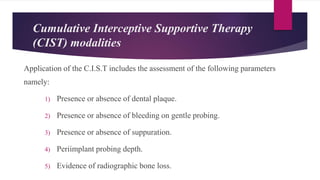
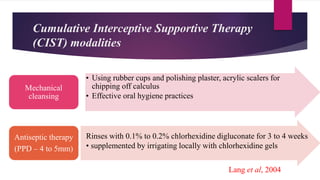
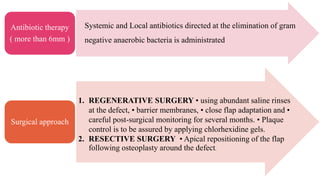
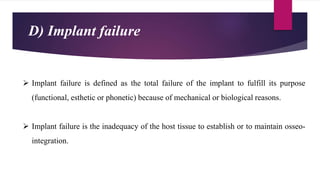
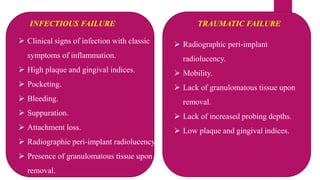
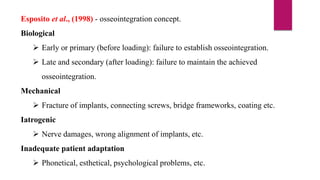
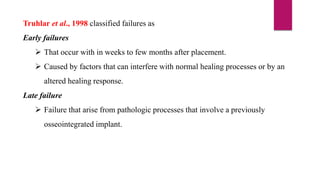
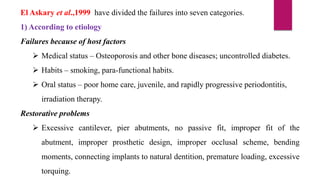
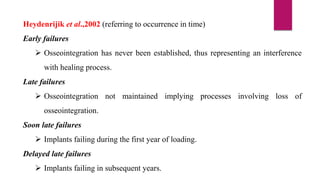
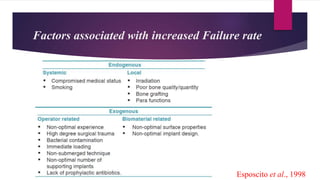
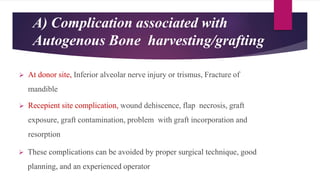
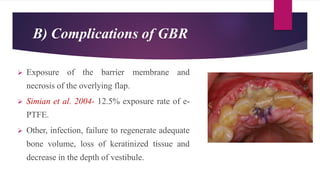
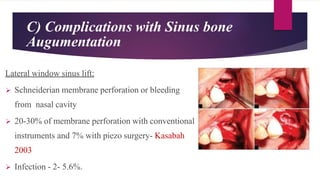
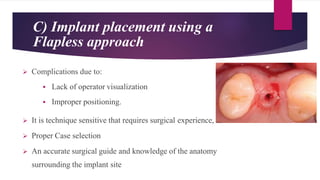
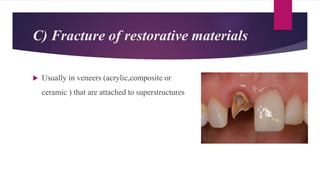
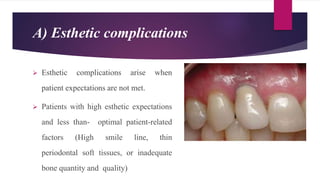
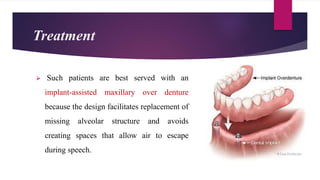
This document discusses implant complications and failures. It begins with an introduction to dental implants and their success. It then defines key implant terms and outlines factors that can influence outcomes. The document details various types of implant complications including surgical, biological, augmentation-related, placement/loading protocol, and prosthetic/mechanical. It provides examples of specific complications within each category such as hemorrhaging, neurosensory disturbances, peri-implantitis, screw loosening, and esthetic problems. The document concludes with a section on implant removal.