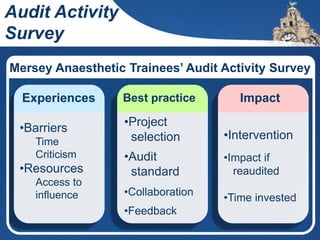
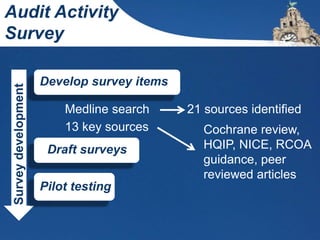
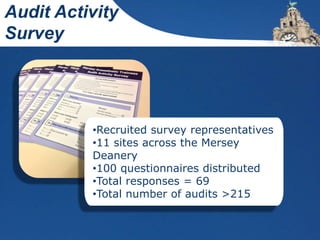
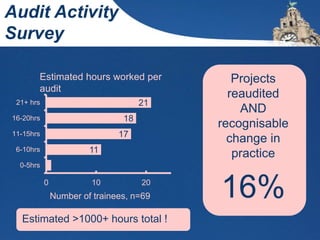
1. The document describes a survey of anaesthetic trainees in Merseyside that found they collectively spent over 1000 hours on audits but only 16% resulted in recognizable practice changes.
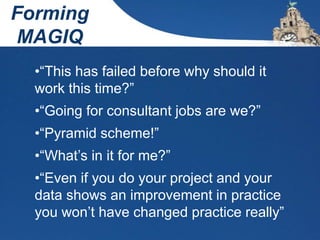
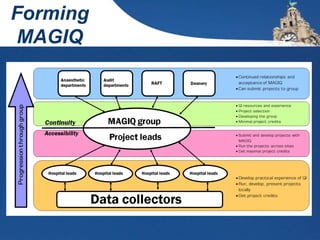
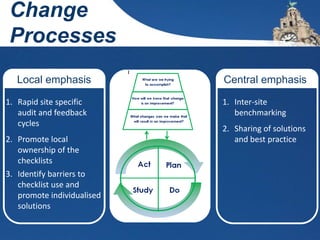
2. It then outlines the formation of MAGIQ (Mersey Anaesthetic Group for Improving Quality) to help trainees collaborate on quality improvement projects and overcome barriers like lack of time, resources and support.
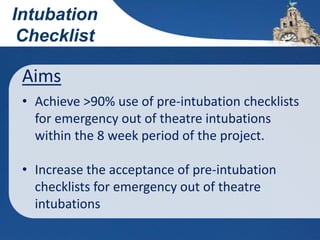
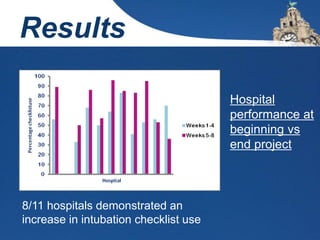
3. One such project was a Mersey-wide initiative to increase the use of pre-intubation checklists, which through rapid audit and feedback across 11 hospitals was able to increase checklist use from 51% to 87% over 8 weeks.