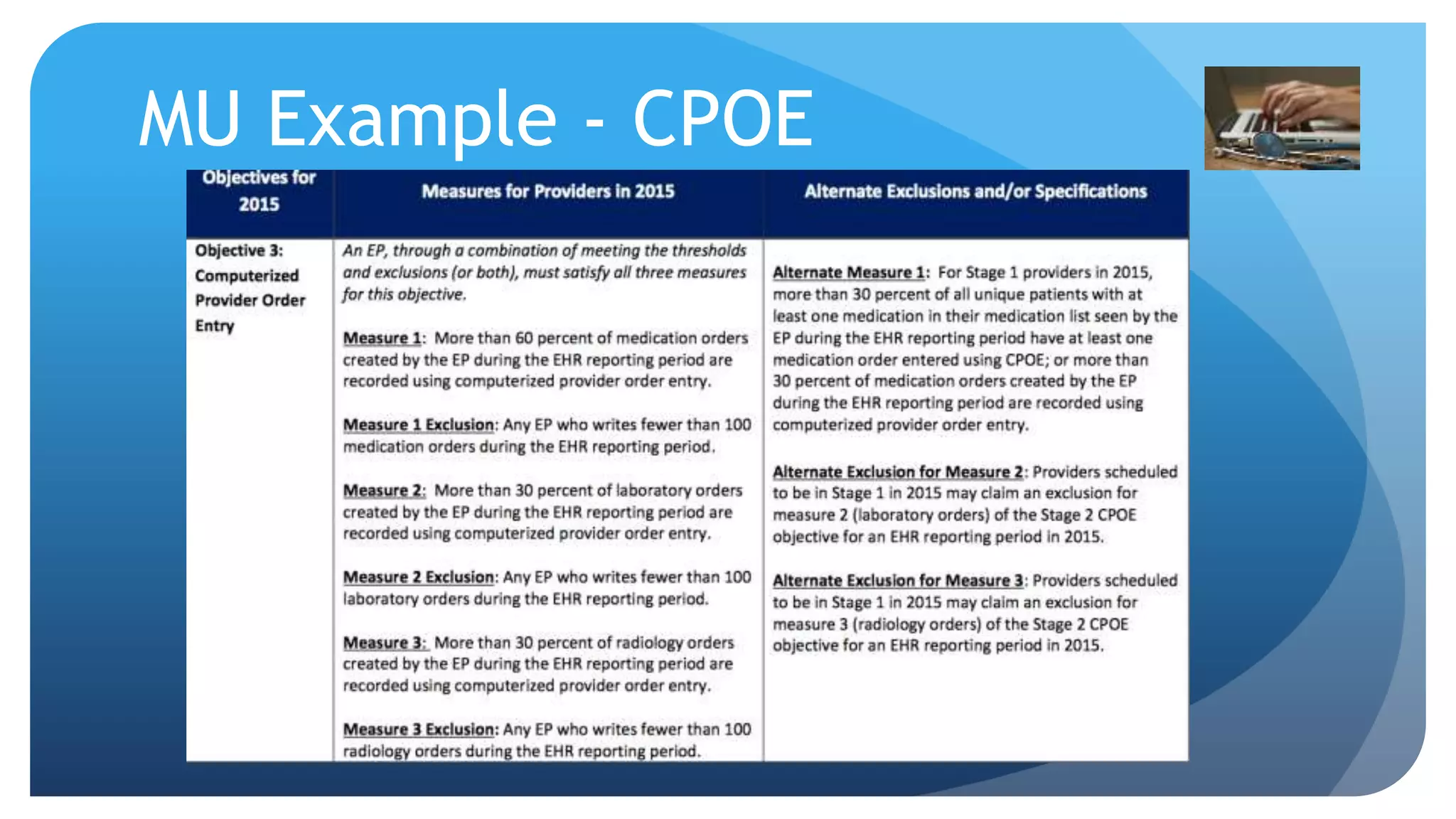
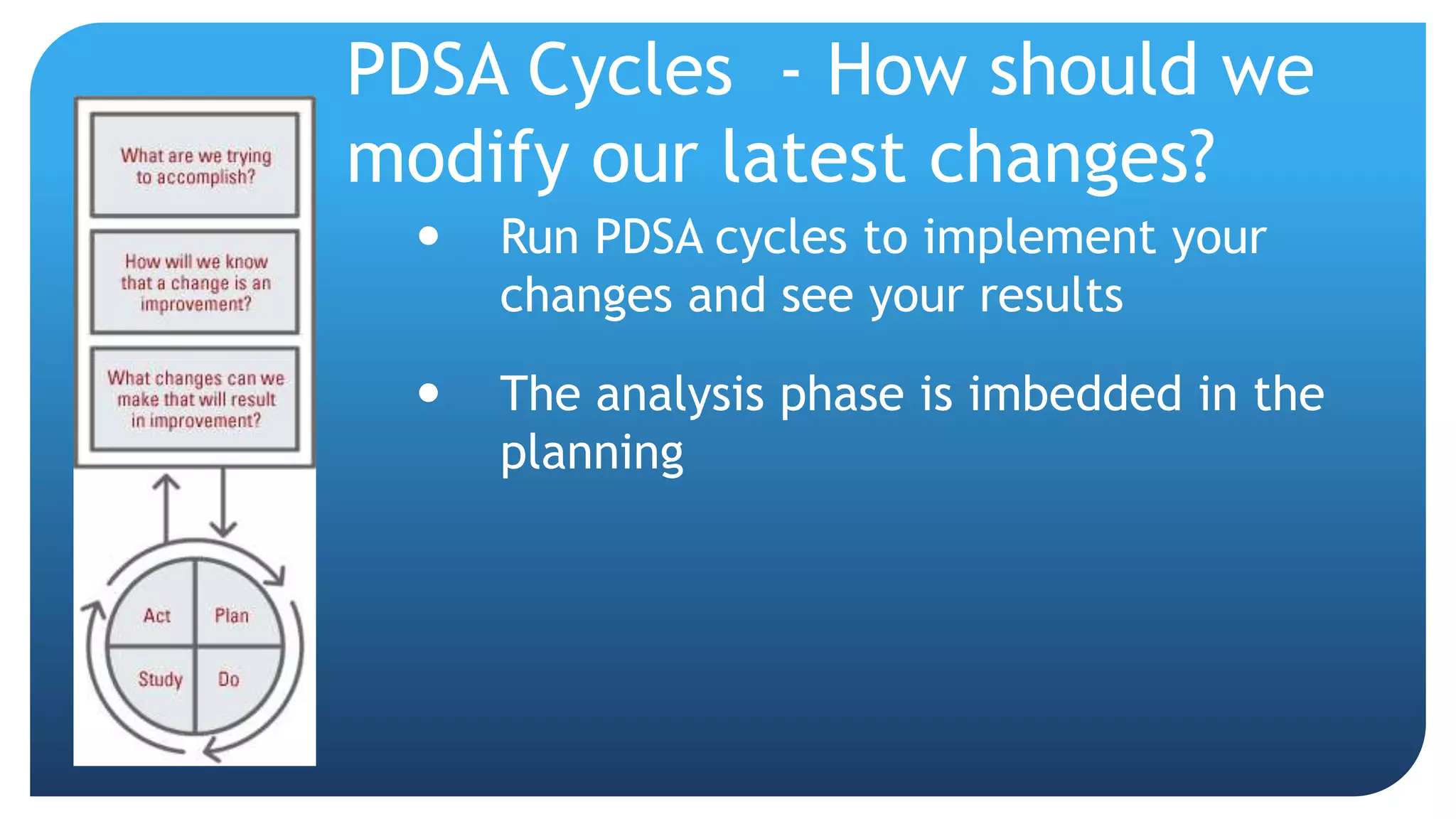
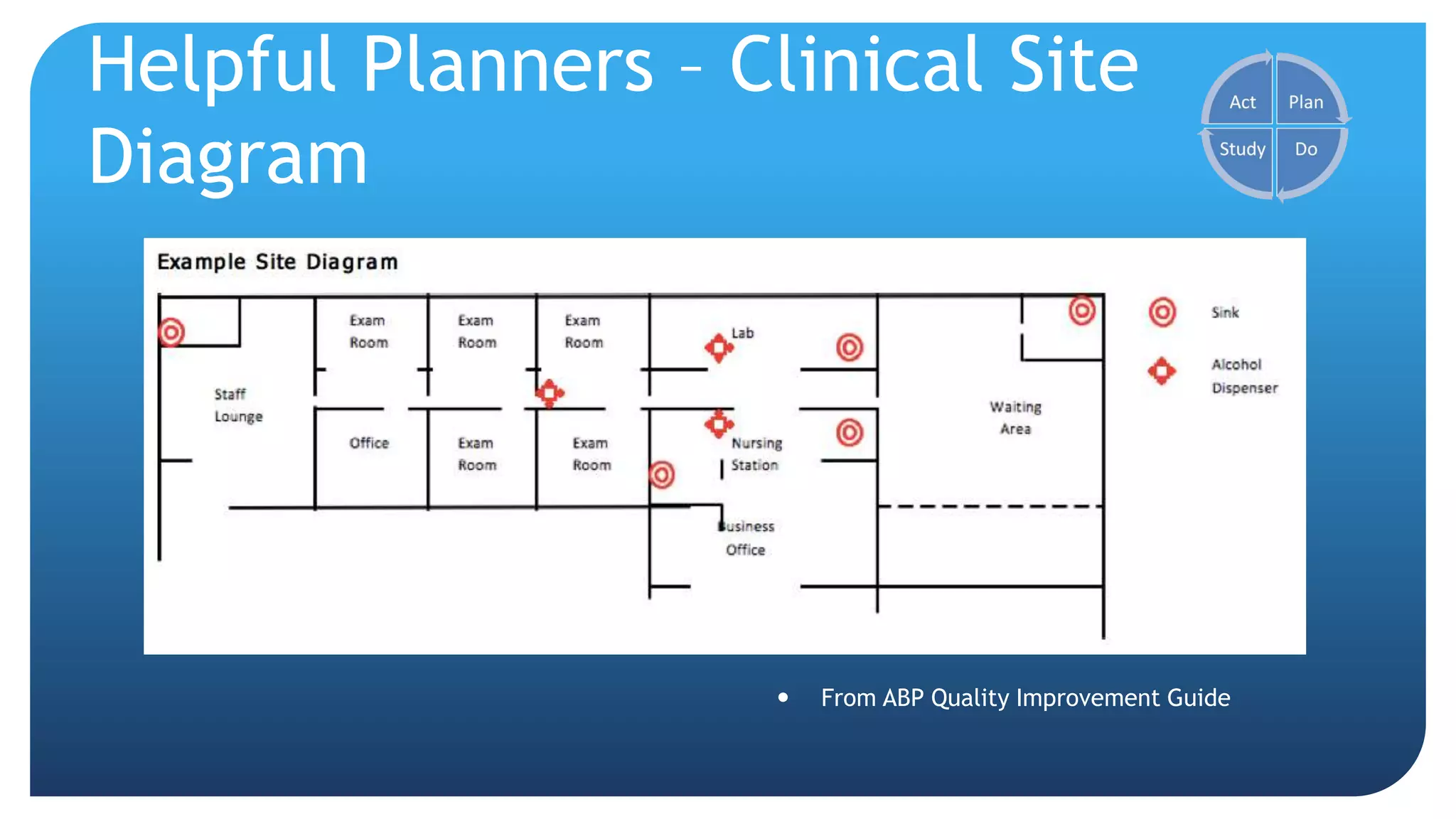
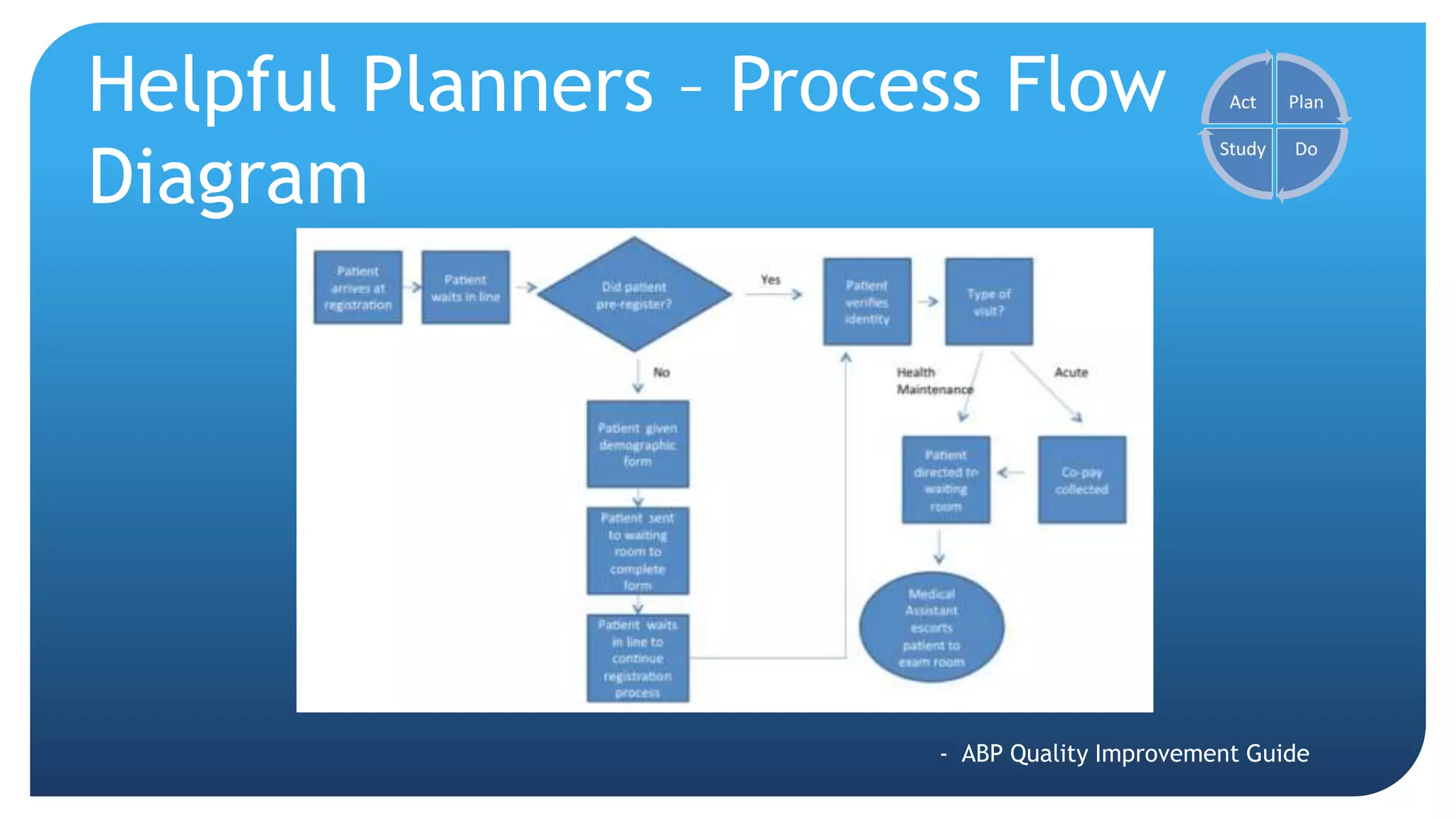
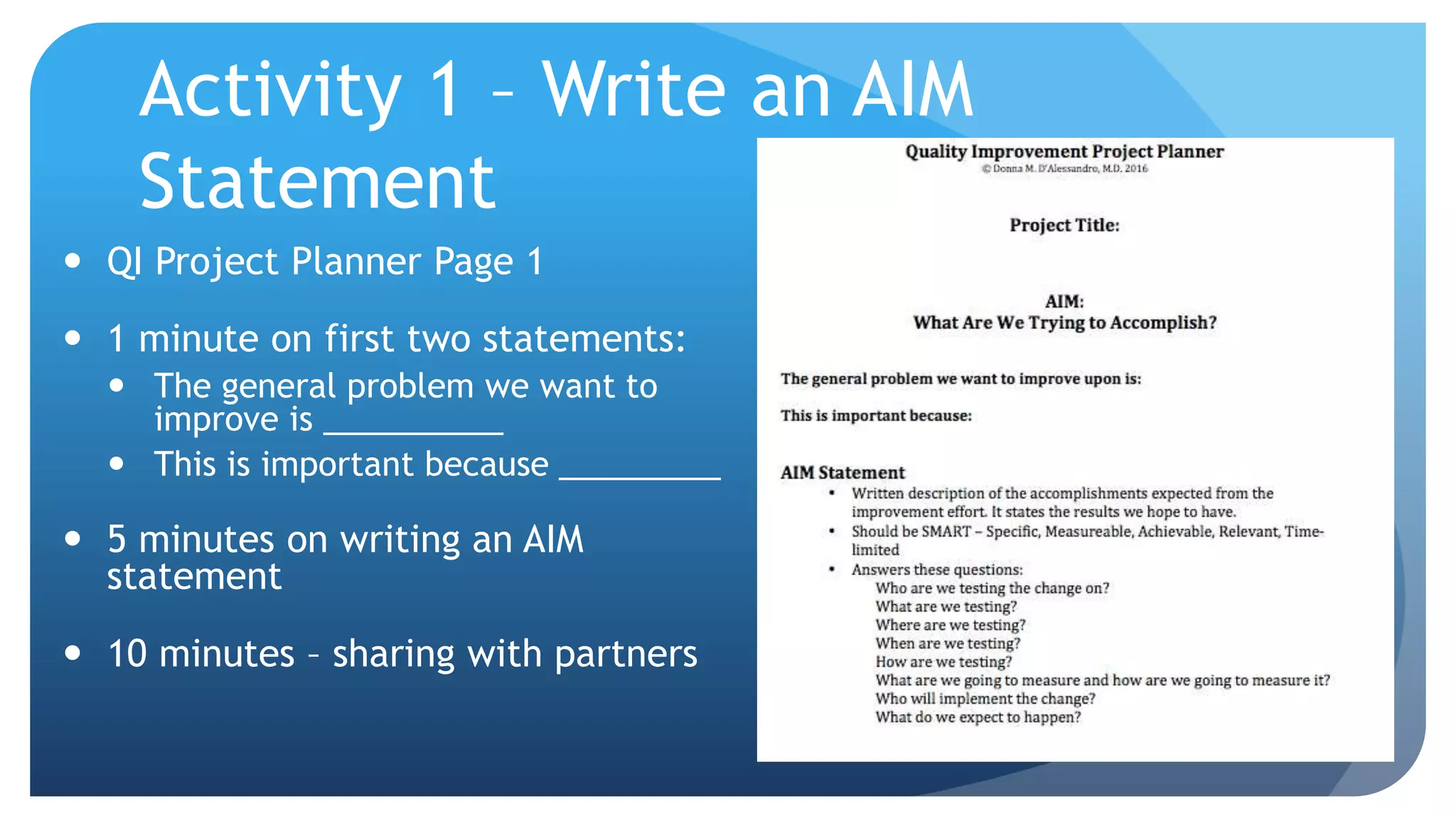
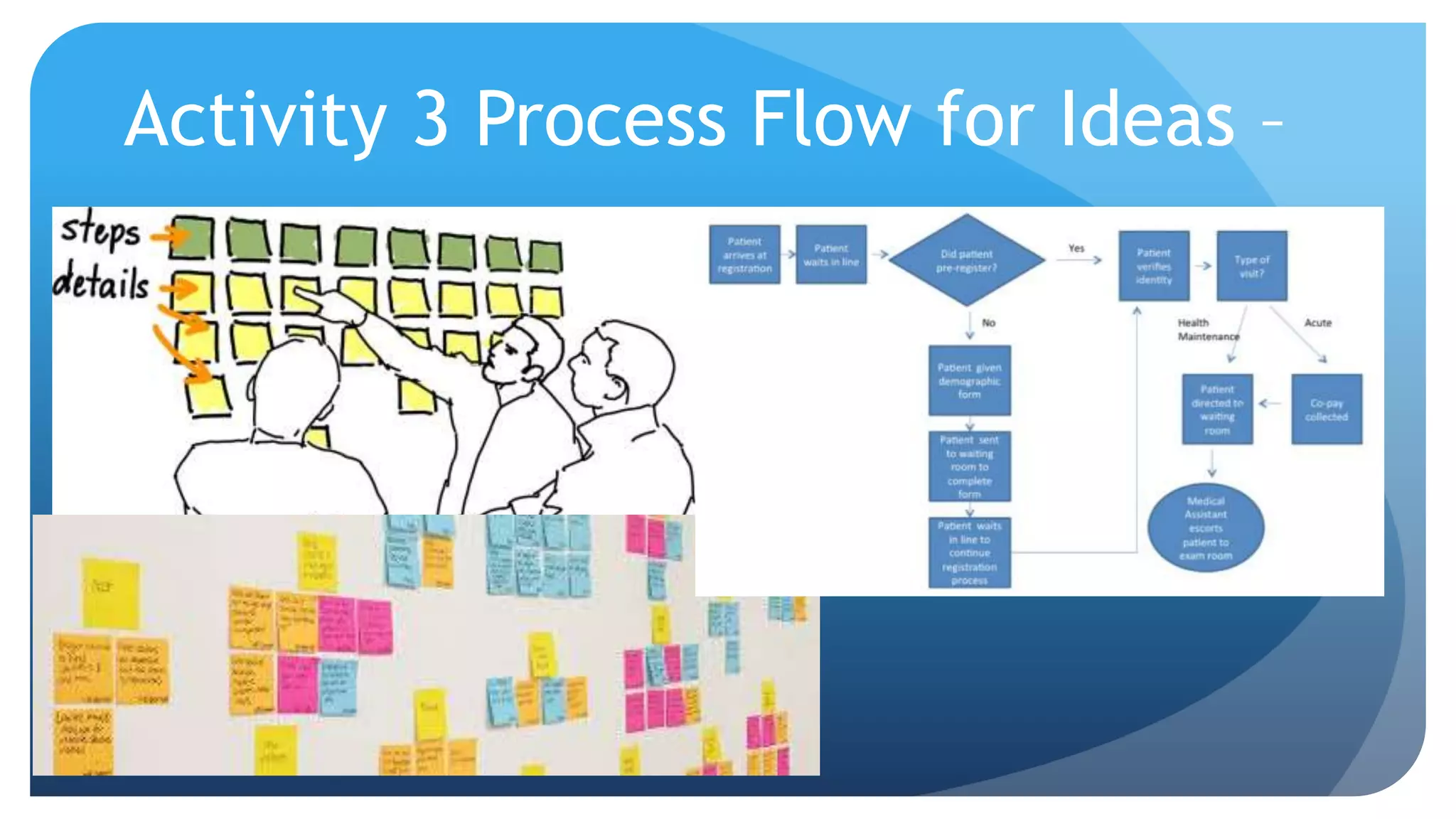
This document summarizes a presentation about Maintenance of Certification (MOC), quality improvement using electronic medical records (EMRs), and developing quality improvement projects. The presentation discusses how MOC can integrate professional competency maintenance with EMR-based quality improvement programs. It outlines the four parts of MOC and various pathways to fulfill the requirements. It also explains how EMRs can be leveraged as tools for quality improvement through functions like clinical decision support, computerized order entry, and reporting quality measures. The document provides guidance on developing a quality improvement project, including writing an aims statement and measure, creating a process flow, and planning the project timeline and team.