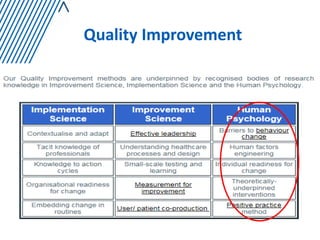
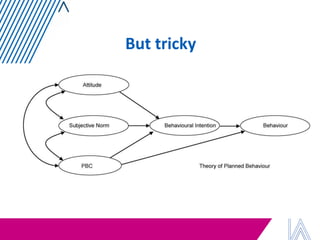
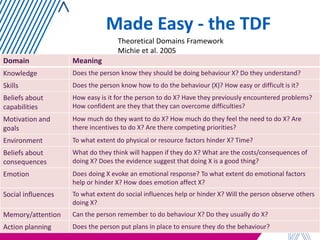
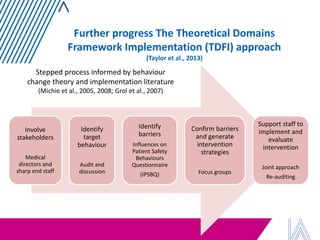
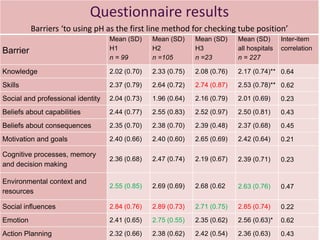
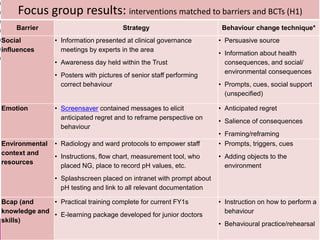
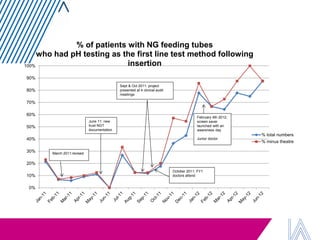
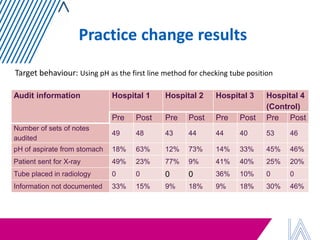
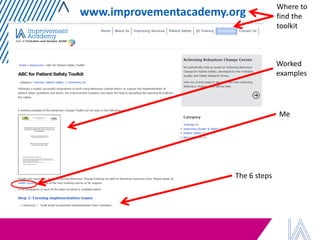
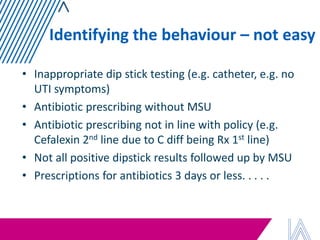
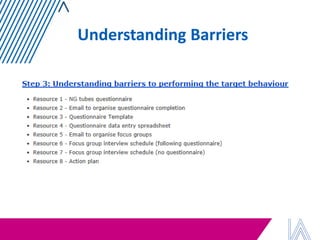
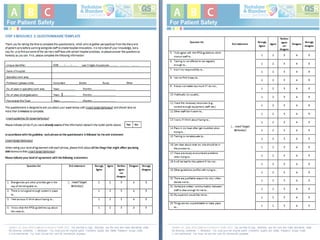
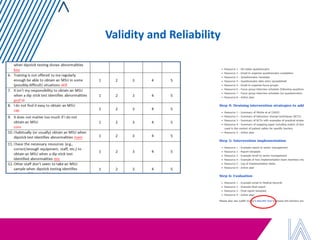
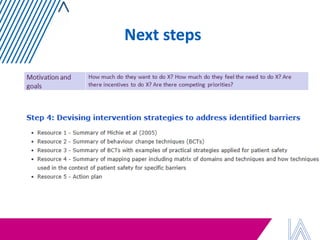
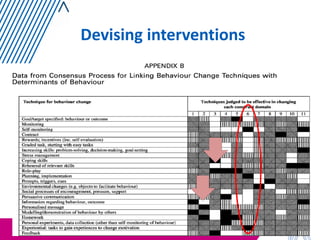
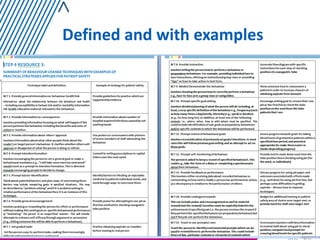
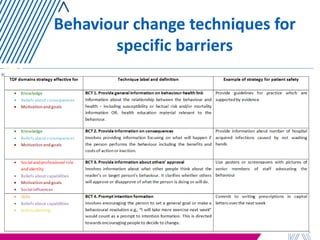
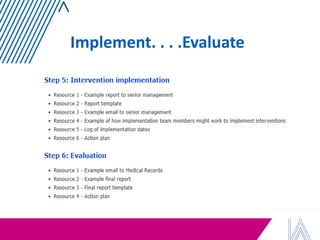
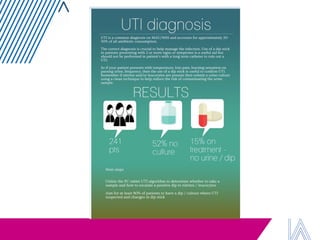
The document discusses strategies for achieving behavior change in patient safety, emphasizing the importance of assessing individual barriers and tailoring interventions based on theoretical frameworks. It outlines how psychological theories can enhance the effectiveness of behavior change techniques, as well as provides examples of barriers and suggested strategies from focus group results. Theoretical frameworks, such as the Theoretical Domains Framework, guide the development and implementation of interventions aimed at improving compliance with patient safety measures.