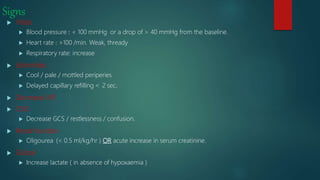
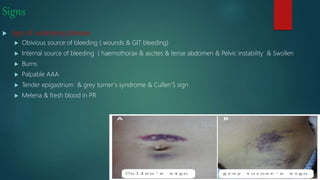
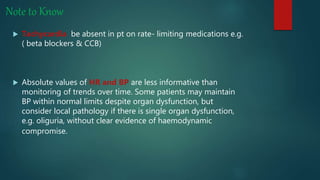
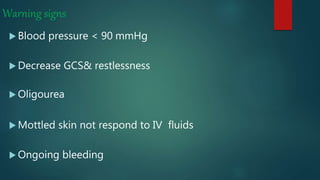
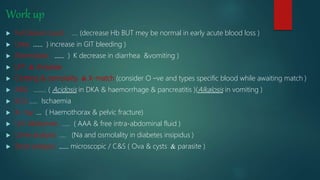
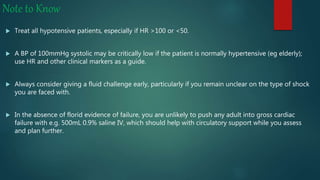
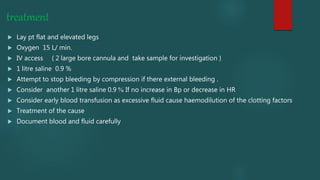
The document discusses shock, particularly hypovolemic shock, emphasizing its causes, symptoms, and vital signs related to decreased tissue perfusion. It outlines diagnostic and treatment protocols, including the importance of monitoring trends in blood pressure and heart rate, while considering early interventions like fluid resuscitation. Additionally, it highlights the risks of excessive fluid administration and the concept of permissive hypotension during management.