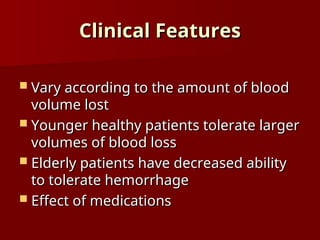
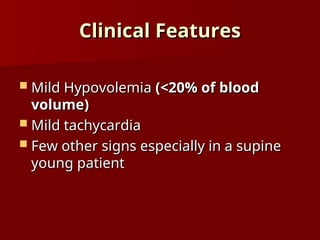
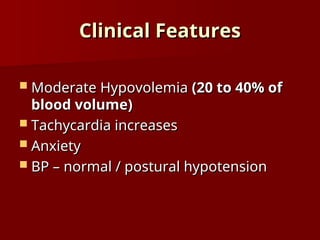
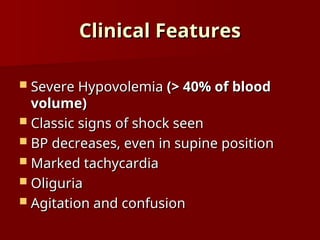
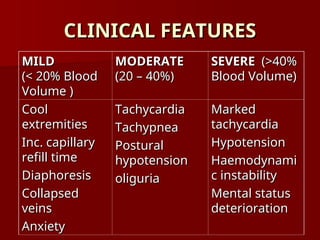
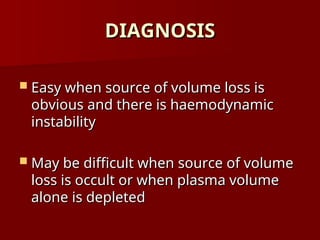
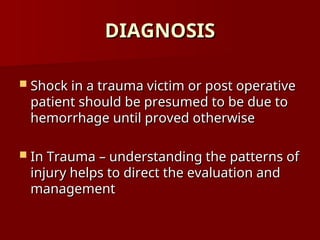
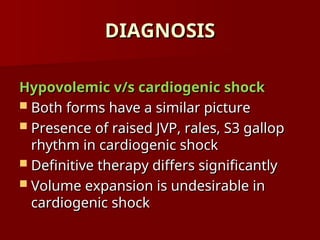
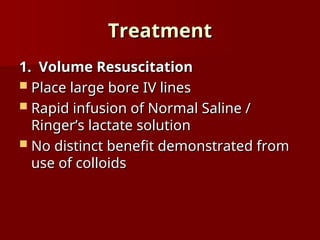
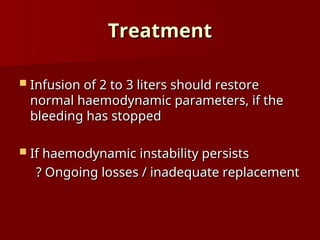
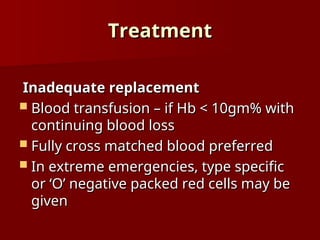
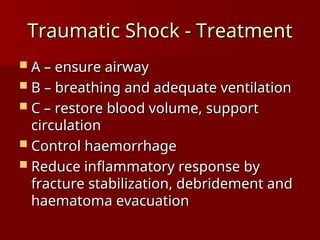
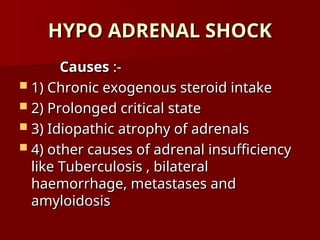
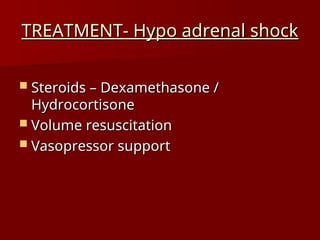
Shock is a clinical syndrome characterized by inadequate tissue perfusion leading to tissue hypoxia, cellular dysfunction, and injury. It has different types, including hypovolemic, cardiogenic, septic, neurogenic, and hypo adrenal shock, with clinical features evolving based on the volume of blood loss. Treatment focuses on volume resuscitation, control of bleeding, and supportive measures, as untreated hypovolemia can lead to irreversible cell injury and death.