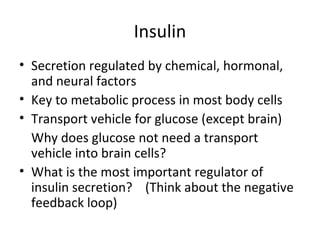
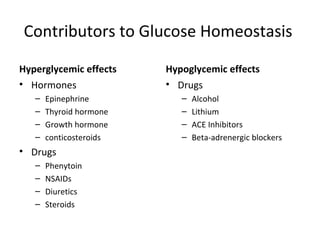
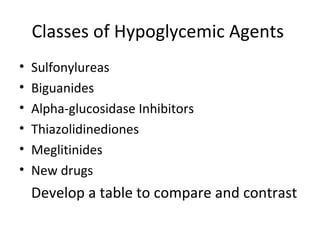
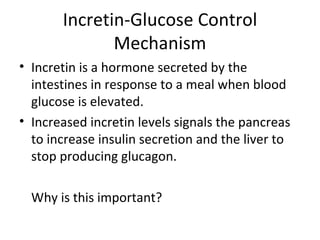
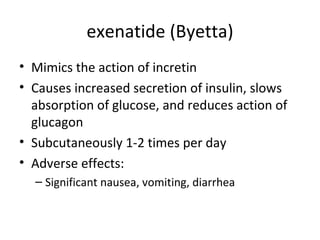
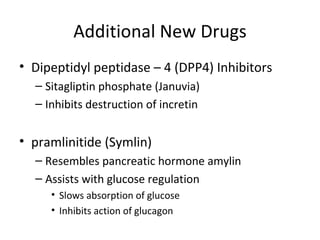
The document discusses the endocrine system and drugs for diabetes mellitus. It covers the functions of the pancreas and insulin, the two main types of diabetes, and pharmacotherapy options for managing blood glucose levels. Type 1 diabetes is treated primarily with insulin therapy to replace deficient insulin. Type 2 diabetes is usually initially managed through oral hypoglycemic agents and lifestyle changes, though some patients may eventually require insulin. Newer drug classes like incretin mimetics and DPP-4 inhibitors work by augmenting the body's natural incretin response to help regulate glucose levels. Nursing considerations for all diabetic pharmacotherapy include medication administration, monitoring for side effects like hypoglycemia, and providing education to patients.