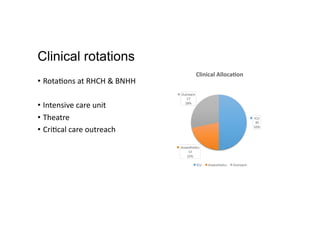
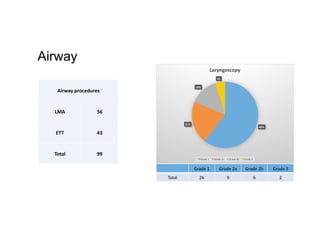
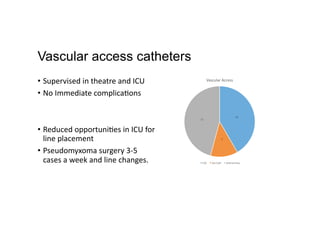
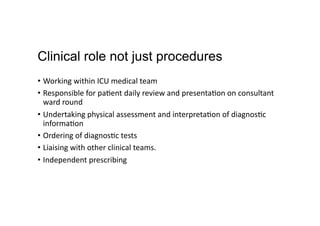
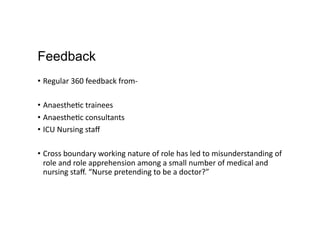
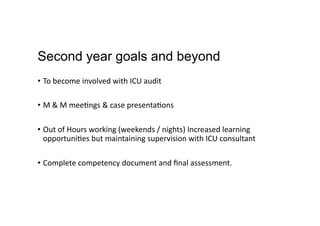
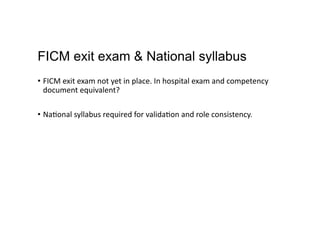
This document summarizes Lee Berry's training and experience as an Acute Care Practitioner (ACP). It outlines their educational background and clinical rotations in intensive care, anesthesia, and outreach. It also describes the practical procedures Lee performed such as intubation, vascular access, and prescribing. Feedback was generally positive but some misunderstanding of the ACP role was encountered. Long term goals include increased responsibility and competency in the intensive care unit.