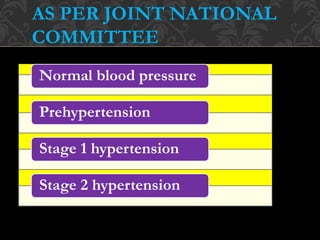
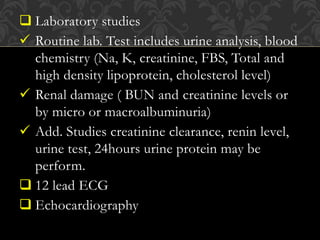
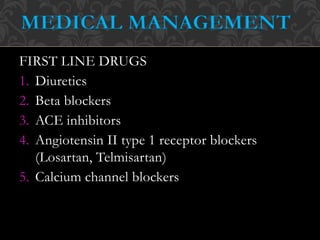
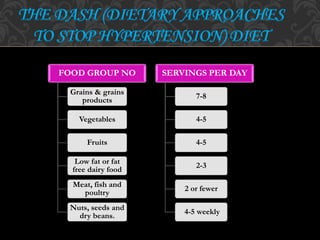
The document discusses hypertension, defining it as elevated blood pressure with specific systolic and diastolic thresholds. It outlines the causes, risk factors, classifications, symptoms, and treatment options, including both first-line and second-line medications. The management strategies also emphasize lifestyle changes, dietary modifications, and nursing considerations for effective control of high blood pressure.