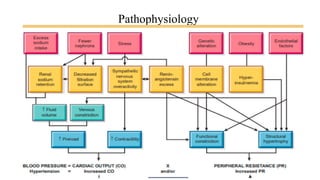
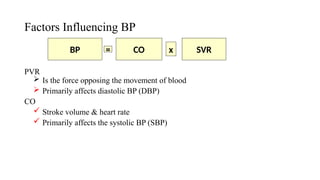
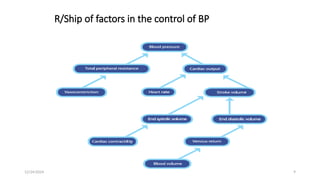
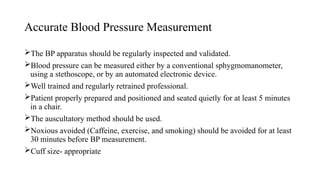
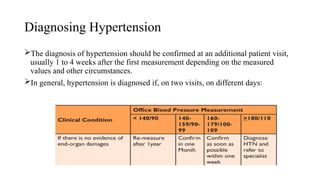
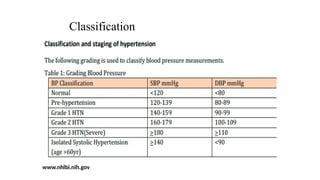
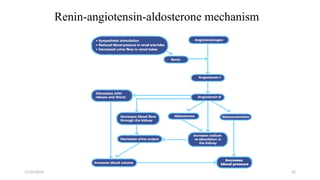
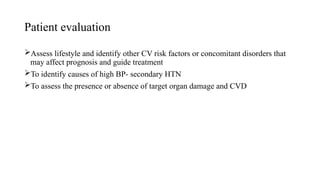
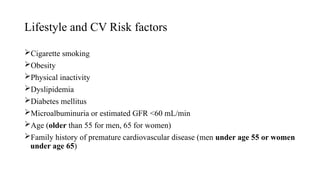
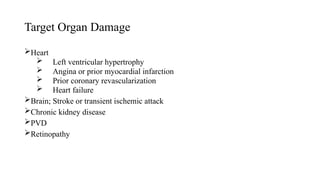
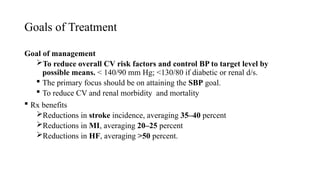
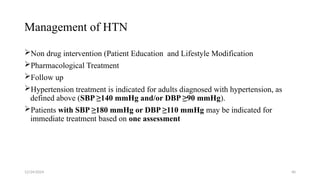
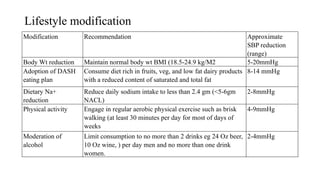
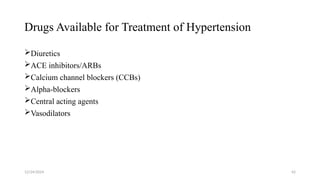
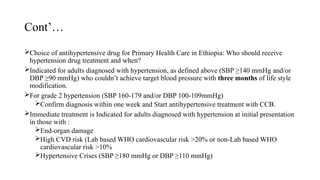
Hypertension, commonly known as the 'silent killer,' affects approximately 30% of adults globally and contributes to over 7 million deaths annually. It is characterized by persistently elevated blood pressure (≥140/90 mmHg) and has various causes, classifications, and treatment strategies, including lifestyle modifications and medications. The management of hypertension aims to reduce cardiovascular risks and prevent complications such as heart disease, stroke, and kidney failure.