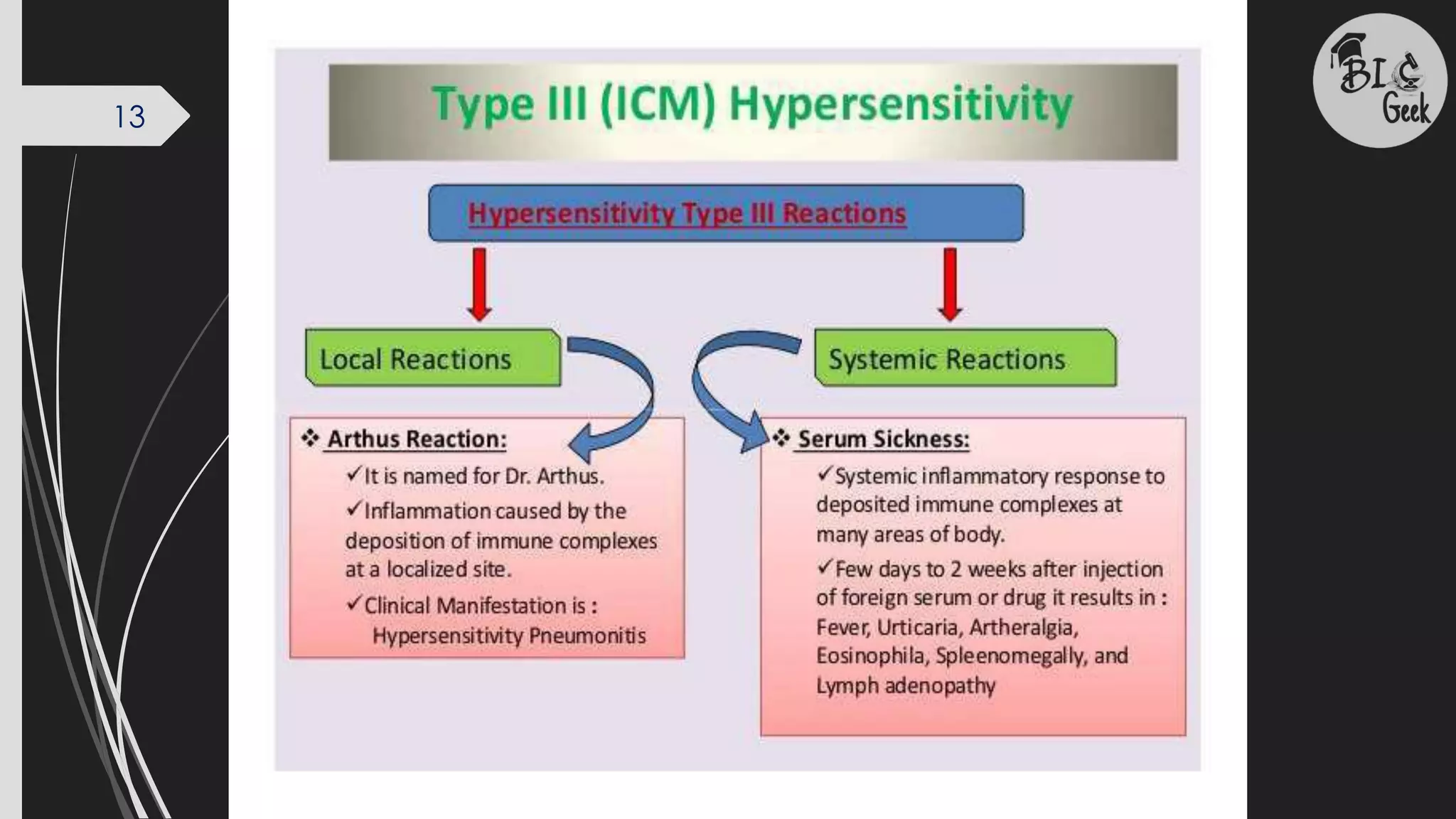
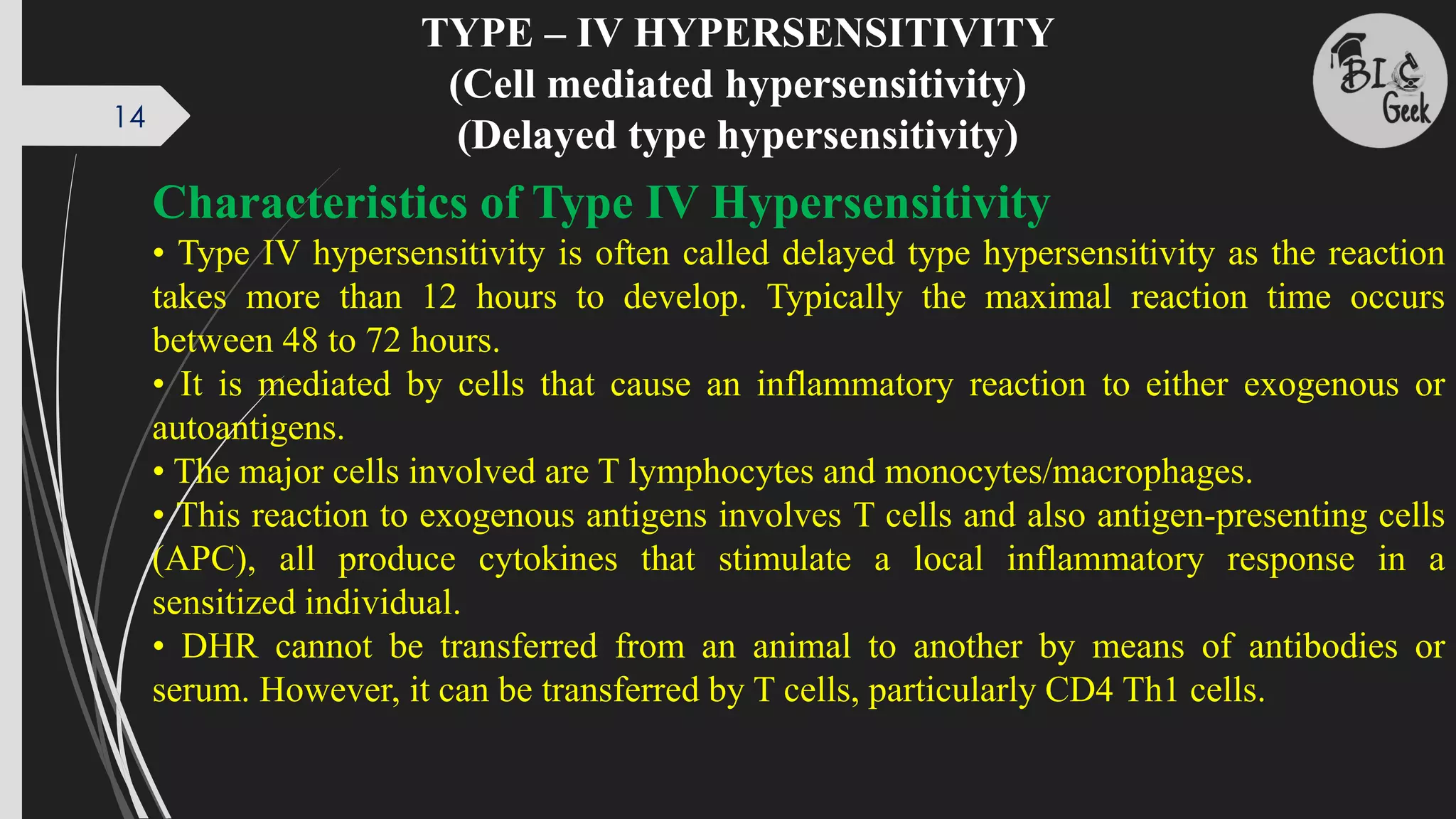
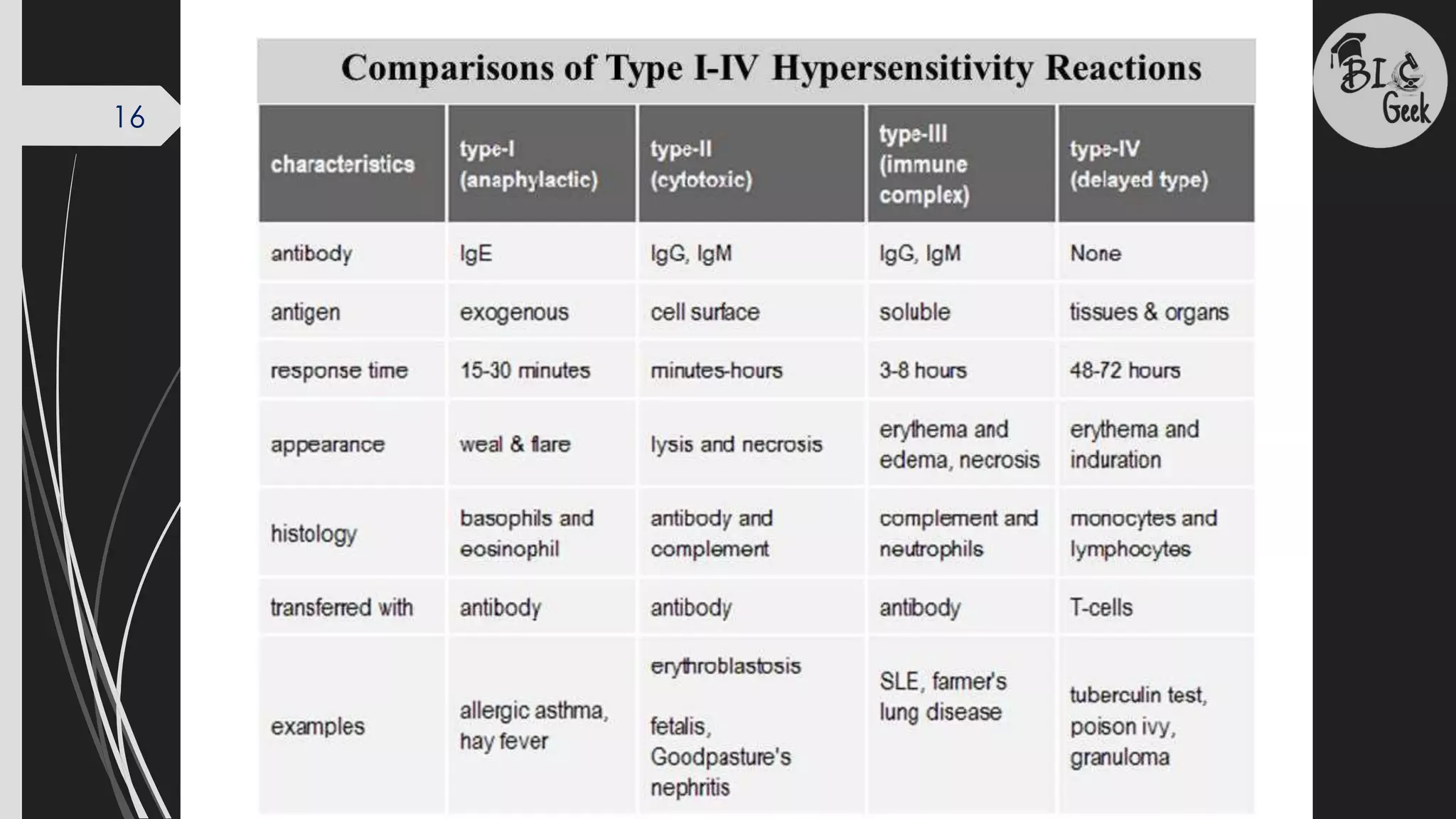
The document provides a comprehensive overview of hypersensitivity reactions, categorizing them into four types: Type I (immediate hypersensitivity), Type II (antibody-mediated cytotoxic hypersensitivity), Type III (immune complex-mediated hypersensitivity), and Type IV (cell-mediated hypersensitivity). Each type is characterized by its underlying mechanisms, timing, and effects on the body, including details on symptoms, cellular involvement, and relevant diagnostic tests. Type I and II emphasize responses mediated by antibodies, while Type III involves immune complexes in tissue damage, and Type IV is a delayed response mediated by T cells.