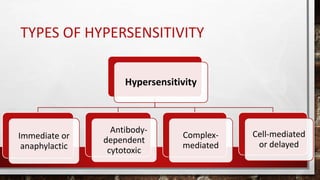
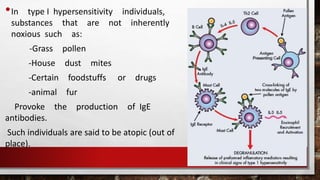
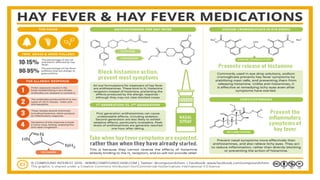
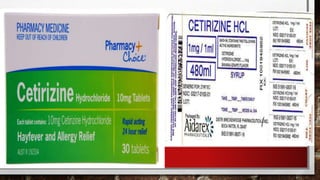
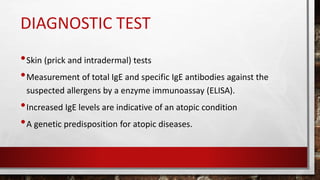
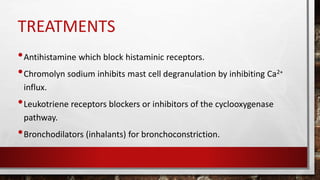
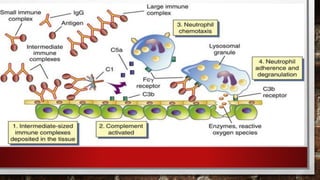
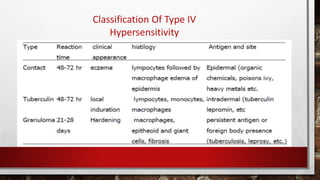
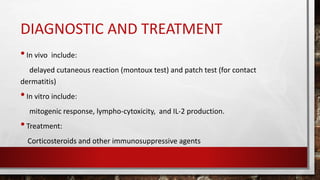
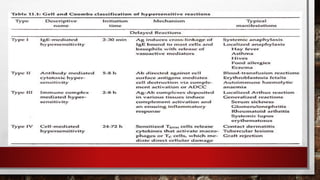
This document summarizes the four main types of hypersensitivity reactions: Type I (immediate or anaphylactic), Type II (antibody-dependent cytotoxic), Type III (complex-mediated), and Type IV (cell-mediated or delayed). It provides details on the mechanisms, examples, diagnostic tests and treatments for each type of hypersensitivity reaction.