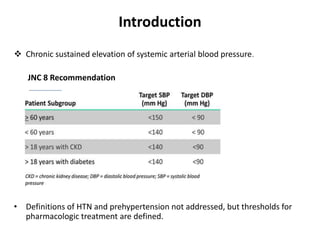
This document discusses the pharmacotherapy of hypertension. It begins by defining hypertension and discussing its physiological regulation. It then covers the principles of antihypertensive therapy, classifying drugs by their primary mechanisms of action. The main drug classes discussed are diuretics, sympatholytics, calcium channel blockers, ACE inhibitors, angiotensin receptor blockers, direct renin inhibitors, and vasodilators. For each class, it describes the pharmacological effects, therapeutic uses, dosing, and adverse drug reactions. It concludes by discussing lifestyle modifications and strategies for dosing antihypertensive drugs according to JNC8 guidelines.










![• Amiloride [K+-sparing diuretic] has some efficacy in lowering BP.
• Spironolactone, lowers BP but has significant ADRs, especially in men
(e.g., erectile dysfunction, gynecomastia, benign prostatic hyperplasia).
• Should be used cautiously with frequent measurements of K+
concentrations in plasma.
• Renal insufficiency is a relative contraindication to the use of K+-sparing
diuretics.
• Concomitant use of an ACEI or an ARA magnifies risk of hyperkalemia.](https://image.slidesharecdn.com/htn-170223083209/85/Pharmacotherapy-Management-of-Hypertension-JNC-8-guidelines-13-320.jpg)








![• Used in hypertensive for diagnosis of pheochromocytoma. [lack of
suppression of plasma concn. of NE to >500 pg/mL 3 hours after oral dose
of 0.3 mg of clonidine suggests tumor presence].
• ADRs-
• Sedation, xerostomia (parotid gland swelling and pain), postural
hypotension, sleep disturbances, restlessness, depression, bradycardia
and sinus arrest, contact dermatitis(transdermal).
• Sudden discontinuation of clonidine α2 adrenergic agonists may cause a
withdrawal syndrome.](https://image.slidesharecdn.com/htn-170223083209/85/Pharmacotherapy-Management-of-Hypertension-JNC-8-guidelines-22-320.jpg)


















