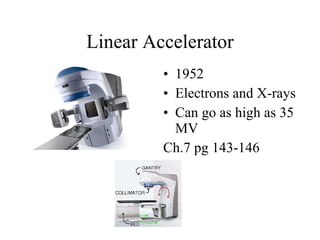
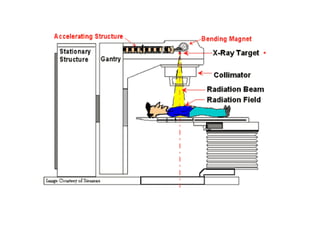
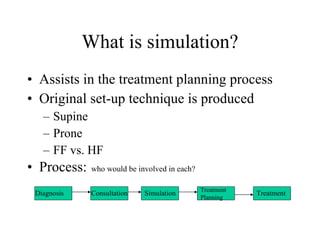
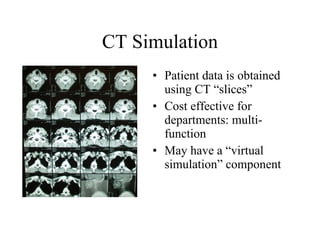
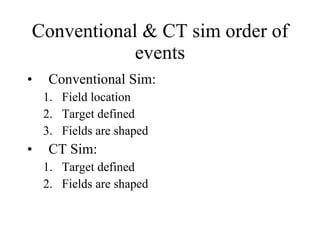
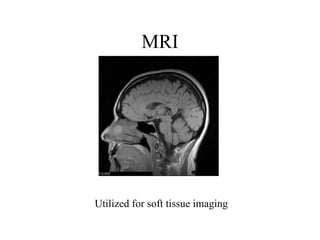
The document provides a brief history of radiation therapy and x-rays, including their discovery in the late 19th century, and developments in equipment over time. It discusses early radiation therapy methods like orthovoltage and kilovoltage treatments. It also summarizes linear accelerators and how they improved upon older cobalt-60 and betatron technology to allow higher energy photon beams for treating deeper tumors. Simulation equipment is covered, comparing conventional versus CT-based simulation and how various imaging modalities can aid treatment planning.