Ssd calculations
•Download as PPT, PDF•
0 likes•1,948 views
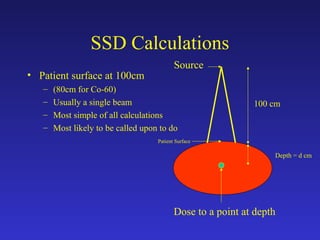
This document discusses SSD calculations for radiation therapy treatment planning. It provides examples of calculating monitor units (MUs) needed to deliver a prescribed dose to different depths using various field sizes and source-to-surface distances (SSDs), accounting for factors like percent depth dose (PDD), inverse square, scatter, and blocking. It also gives an example of calculating the dose to the depth of maximum dose (dmax) given a prescribed dose to another depth using the ratio of PDD values.
Report
Share
Report
Share
Recommended
Sad calculations

The document discusses the calculation of monitor units (MU) for radiation therapy treatment plans using the standard equation of prescribed dose multiplied by various correction factors. It provides examples of calculating MUs for different treatment scenarios, including different depths, field sizes, source-to-axis distances (SAD), and weighted beam arrangements. The key factors involved are reference dose rate, inverse square correction, collimator scatter, phantom scatter, tissue maximum ratio (TMR), and other applicable corrections.
Dosimetric calculations

This document provides information on dosimetric calculations for radiation therapy. It discusses key concepts like percent depth dose (PDD) and tissue maximum ratio (TMR) which are used to calculate dose for non-isocentric and isocentric setups, respectively. Factors like collimator scatter, phantom scatter, and beam modifiers are also covered. The document outlines the basic principles and provides examples of SSD and SAD calculations.
Commissioning of Truebeam LINAC

The document provides details about the acceptance testing and commissioning of a new TrueBeam linear accelerator installed at the facility. Some key details include:
- The machine was installed in an existing bunker previously occupied by a Siemens Primus Plus with additional shielding added.
- Acceptance testing verifies a small subset of beam data based on manufacturer guidelines to check specifications, while commissioning involves comprehensive beam measurements and treatment planning system configuration.
- Beam data measurements included depth doses, profiles, output, symmetry, flatness, and other dosimetric parameters which were analyzed and entered into the treatment planning system.
- Electron and photon beam energies and characteristics were evaluated to ensure they met tolerance limits. Other
Flattening filter Free

1. The document discusses commissioning parameters for flattening filter free (FFF) photon beams from a linear accelerator, including profile normalization methods, dosimetric field size, penumbra, and slope.
2. Profile normalization can be done using the inflection point or renormalization value to compare FFF and flattened beams. Dosimetric field size is measured as the 50% dose width. Penumbra is defined as the 20-80% distance for FFF beams after normalization.
3. Slope describes the peak shape of FFF profiles, and flatness/unflatness parameters are discussed to characterize beam homogeneity for both FFF and flattened beams.
Isodose lines

Isodose lines represent points of equal absorbed radiation dose on a dose distribution map. They are depicted as curves on isodose charts showing the volumetric and planar variations in absorbed dose. Factors influencing isodose curves include beam quality, field size, source-to-skin distance, beam modifiers like wedges or bolus, and depth. Isodose curves are used in radiation therapy treatment planning to evaluate dose distributions and ensure tumor coverage while sparing surrounding healthy tissues. They provide critical information about the radiation dose profile essential for safe and effective treatment.
EPID AND CBCT ON RADIATION THERAPY

This document discusses various techniques used for treatment verification in radiation therapy. It describes electronic portal imaging devices (EPID) which can be used for daily treatment localization and verification through portal images with little additional dose. Cone beam computed tomography (CBCT) is also discussed, which provides volumetric CT images with submillimeter resolution, allowing verification of patient positioning before treatment. Both EPID and CBCT help ensure the correct radiation dose is delivered to the intended target volume.
TSET

Total skin electron therapy (TSET) is used to treat cutaneous T-cell lymphoma by delivering a uniform dose of radiation to the entire skin surface while sparing underlying organs. It requires large electron fields over the entire body and precise dosimetry. The most common technique uses six electron beams arranged at 60 degree intervals to provide circumferential coverage. Proper field design and calibration are needed to achieve uniform dose across irregular body surfaces and minimize dose from bremsstrahlung x-rays.
Sealed radionuclides

Sealed radioactive sources are radioactive material permanently sealed in a capsule. Common sealed sources used in brachytherapy include cesium-137, iridium-192, cobalt-60, iodine-125, gold-198, and radium-226. Each isotope has different properties such as half-life, photon energy emitted, and exposure rate constant. Sources are constructed of radioactive material encapsulated in stainless steel, gold or platinum capsules to prevent leakage and are available in various geometries like seeds, ribbons, or tubes to suit different clinical applications in brachytherapy.
Recommended
Sad calculations

The document discusses the calculation of monitor units (MU) for radiation therapy treatment plans using the standard equation of prescribed dose multiplied by various correction factors. It provides examples of calculating MUs for different treatment scenarios, including different depths, field sizes, source-to-axis distances (SAD), and weighted beam arrangements. The key factors involved are reference dose rate, inverse square correction, collimator scatter, phantom scatter, tissue maximum ratio (TMR), and other applicable corrections.
Dosimetric calculations

This document provides information on dosimetric calculations for radiation therapy. It discusses key concepts like percent depth dose (PDD) and tissue maximum ratio (TMR) which are used to calculate dose for non-isocentric and isocentric setups, respectively. Factors like collimator scatter, phantom scatter, and beam modifiers are also covered. The document outlines the basic principles and provides examples of SSD and SAD calculations.
Commissioning of Truebeam LINAC

The document provides details about the acceptance testing and commissioning of a new TrueBeam linear accelerator installed at the facility. Some key details include:
- The machine was installed in an existing bunker previously occupied by a Siemens Primus Plus with additional shielding added.
- Acceptance testing verifies a small subset of beam data based on manufacturer guidelines to check specifications, while commissioning involves comprehensive beam measurements and treatment planning system configuration.
- Beam data measurements included depth doses, profiles, output, symmetry, flatness, and other dosimetric parameters which were analyzed and entered into the treatment planning system.
- Electron and photon beam energies and characteristics were evaluated to ensure they met tolerance limits. Other
Flattening filter Free

1. The document discusses commissioning parameters for flattening filter free (FFF) photon beams from a linear accelerator, including profile normalization methods, dosimetric field size, penumbra, and slope.
2. Profile normalization can be done using the inflection point or renormalization value to compare FFF and flattened beams. Dosimetric field size is measured as the 50% dose width. Penumbra is defined as the 20-80% distance for FFF beams after normalization.
3. Slope describes the peak shape of FFF profiles, and flatness/unflatness parameters are discussed to characterize beam homogeneity for both FFF and flattened beams.
Isodose lines

Isodose lines represent points of equal absorbed radiation dose on a dose distribution map. They are depicted as curves on isodose charts showing the volumetric and planar variations in absorbed dose. Factors influencing isodose curves include beam quality, field size, source-to-skin distance, beam modifiers like wedges or bolus, and depth. Isodose curves are used in radiation therapy treatment planning to evaluate dose distributions and ensure tumor coverage while sparing surrounding healthy tissues. They provide critical information about the radiation dose profile essential for safe and effective treatment.
EPID AND CBCT ON RADIATION THERAPY

This document discusses various techniques used for treatment verification in radiation therapy. It describes electronic portal imaging devices (EPID) which can be used for daily treatment localization and verification through portal images with little additional dose. Cone beam computed tomography (CBCT) is also discussed, which provides volumetric CT images with submillimeter resolution, allowing verification of patient positioning before treatment. Both EPID and CBCT help ensure the correct radiation dose is delivered to the intended target volume.
TSET

Total skin electron therapy (TSET) is used to treat cutaneous T-cell lymphoma by delivering a uniform dose of radiation to the entire skin surface while sparing underlying organs. It requires large electron fields over the entire body and precise dosimetry. The most common technique uses six electron beams arranged at 60 degree intervals to provide circumferential coverage. Proper field design and calibration are needed to achieve uniform dose across irregular body surfaces and minimize dose from bremsstrahlung x-rays.
Sealed radionuclides

Sealed radioactive sources are radioactive material permanently sealed in a capsule. Common sealed sources used in brachytherapy include cesium-137, iridium-192, cobalt-60, iodine-125, gold-198, and radium-226. Each isotope has different properties such as half-life, photon energy emitted, and exposure rate constant. Sources are constructed of radioactive material encapsulated in stainless steel, gold or platinum capsules to prevent leakage and are available in various geometries like seeds, ribbons, or tubes to suit different clinical applications in brachytherapy.
TISSUE PHANTOM RATIO - THE PHOTON BEAM QUALITY INDEX

TPR(20,10) is the recommended photon beam quality index by IAEA TRS-398 for megavoltage clinical photons generated by linear accelerators. This presentation goes through the basics of Tissue Phantom Ratio (TPR).
Importance of Planning CT Simulation(3D) in Radiothrapy/Radiation oncology.

CT simulation is an important part of the radiotherapy planning process. It allows for 3D visualization of patient anatomy using CT scans. Various immobilization devices are used to accurately position the patient for treatment planning and delivery. The summary describes the key steps in CT simulation including patient setup using immobilization devices, obtaining CT images with appropriate parameters, and noting important details in the patient record for their specific diagnosis and treatment area. CT simulation provides critical 3D information to optimize radiotherapy treatment planning.
Exactrac 6D imaging overview

Radiosurgery combines stereotactic techniques and radiation beams to precisely deliver a high dose of radiation to tumors and lesions. The Exactrac system allows for frameless radiosurgery using infrared cameras and x-ray imaging to track internal anatomy and automatically position the patient for treatment without an invasive head frame. Treatment planning involves delineating the target and nearby organs at risk, specifying dose constraints, and optimizing the plan to conform the high dose region to the tumor while sparing surrounding healthy tissue.
Treatment plannings i kiran

Isodose curves depict absorbed dose distributions and variations in volume and planes. They join points of equal dose. Isodose charts show the variation in dose as a function of depth and transverse distance from the central beam axis. Factors like beam energy, field size, and distance affect isodose curve shape through penumbra and dose deposition. Multiple beams are often needed to adequately treat tumors while sparing surrounding tissues. Beam arrangements, weights, and modifiers must be optimized for each plan.
Electron beam therapy

Electron beam therapy uses accelerated electrons to treat superficial tumors. Electrons interact with matter through inelastic collisions that cause ionization and excitation, and elastic collisions that scatter the electrons. This gives electron beams a characteristically sharp dose drop-off beyond the tumor depth. Key applications of electron beams include treatment of skin cancers, chest wall irradiation for breast cancer, and boost doses to lymph nodes.
Beam modification 

This document discusses various beam modification devices used in radiation therapy. It describes the purpose of beam modification as altering the spatial distribution of radiation to better protect normal tissues and achieve uniform dose distribution. Common devices discussed include shielding blocks, wedges, compensators, and bolus. Shielding blocks are used to protect critical structures by blocking radiation to certain areas. Wedges are used to tilt isodose curves for improved dose conformity. Compensators are designed to even out irregular tissue surfaces. Bolus is placed on the skin to reduce the depth of maximum dose. The document provides details on the materials, design considerations, and clinical applications of these various beam modification tools.
Total skin electron irradiation 

Total skin electron irradiation ppt
Rupon Bhowmik
Dept of Medical physics & biomedical engineering,dhaka
Interstitial BT Principles

This document provides an overview of interstitial brachytherapy principles and concepts. It discusses the history and evolution of brachytherapy sources from radium to modern radioactive sources like iridium-192. Key concepts covered include dose rate calculations, implant systems like the Paris system, and factors that influence dose distribution from a radioactive source like distance, absorption and scattering. The document also describes temporary and permanent brachytherapy sources and different methods of source application including preloading, afterloading and remote afterloading.
Radioisotopes and dose rates used for brachytherapy

Radioisotopes and dose rates used for brachytherapy
This is the seminar about different radioisotopes used in brachytherapy beginning from radium to iradium and different dose rates, low dose rate, high dose rate used in brachytherapy. The significance of different dose rates and its radiobiology along with the clinical results.
Dosimetric Evaluation of High Energy Electron Beams Applied in Radiotherapy

Electron-beam therapy: is used to treat superficial tumors at a standard 100 cm source-to-surface distance (SSD). Characteristics of electron beams from an Elekta PreciseTM linear accelerator are presented at a nominal SSD of 100 cm. However, certain clinical situations require the use of an extended SSD. The effects of extended source-to-surface distance (SSD) on the electron beam dose profiles were evaluated for various electron beam energies 6, 8, 10,12 and 15 MeV and the accuracy of various output correction methods was analyzed on an Elekta PreciseTM linear accelerator using a radiation field analyzer (RFA). Effective SSDs was evaluated for field sizes ranging from 6×6, 10×10, 14×14 and 20×20 cm2 for various energies.
Aim of the work
1.Investigate the physical properties of electron beams
at different beam energies.
2.Evaluate the accuracy of dose calculated by
Treatment Planning System (TPS) and measured for
different field configurations.
Beam Directed Radiotherapy - methods and principles

Beam directed radiotherapy aims to deliver a homogenous tumor dose while minimizing radiation to normal tissues. It involves careful patient positioning, immobilization, tumor localization, field selection, dose calculations, and verification. Key steps include using positioning aids and molds to reproducibly position the patient, imaging such as CT to delineate the tumor volume, contouring to define external body outlines, and dose calculations and verification to ensure accurate delivery.
Motion management in Radiation Oncology - 2020

This document discusses various sources of uncertainty and errors in radiation therapy delivery due to patient and target motion. It describes advances in imaging guidance and motion management techniques like 4D imaging, respiratory gating, abdominal compression, and deep inspiration breath hold to minimize the effects of respiratory motion. Real-time tracking methods like RPM and ExacTrac systems are highlighted which allow continuous monitoring of tumor position throughout treatment. Managing respiratory motion remains an important area of focus to ensure accurate radiation delivery.
Isodose curves RADIATION ONCOLOGY

1. Isodose curves represent the dose distribution from radiation beams and are lines connecting points of equal percentage depth dose. They are used to depict the volumetric and planar variations in absorbed dose.
2. The parameters that affect the shape of isodose curves include beam quality, source size, SSD, SDD, field size, and beam modifiers like wedges and flattening filters. Lower beam energy results in greater lateral scatter and more bulging curves.
3. Multiple radiation fields can be combined using appropriate beam weights, sizes, angles and modifiers to deliver a more uniform dose to the tumor while sparing surrounding tissues. Parameters like setup accuracy and plan practicality are also considered.
linac QA.pptx

This document discusses quality assurance parameters and test frequencies for medical linear accelerators. It outlines electrical, mechanical, and dosimetry QA parameters that are tested daily, weekly, monthly, and yearly. Daily tests check parameters that could affect patient positioning, radiation field definition, output constancy, and safety. Weekly tests add checks for beam congruence, flatness, and symmetry. Monthly tests expand to all mechanical and electrical components. Annual tests involve re-calibration and more stringent tolerance levels to establish new baseline values. Tests ensure spatial and dosimetric accuracy within clinically acceptable limits.
Electron Beam Therapy

Updates on Electron Beam Therapy
I) Introduction
II) Central Axis Depth dose distribution
III) Dosimetric parametrics of electron beam
IV) Clinical Considerations of Electron beam therapy
Helical Tomotherapy

The document discusses helical tomotherapy, a form of radiation therapy that uses a rotating x-ray beam. It summarizes a study of 150 patients treated with tomotherapy between 2006-2007 for reasons such as complex tumor geometry or need for image guidance. Setup corrections were often needed based on pretreatment MV CT scans. Treatment times were typically under 25 minutes with minimal increases over time. Tomotherapy allows conformal dose distributions and image-guided radiation for difficult cases near critical organs.
Dose volume histogram

This document discusses dose-volume histograms (DVHs) which are used to analyze and compare radiation dose distributions in radiotherapy treatment planning. It describes how DVHs are generated by counting the number of voxels receiving different dose levels. DVHs can be displayed cumulatively or differentially and show the volume of structures receiving particular doses. The document outlines some limitations of DVHs including their insensitivity to small hot or cold spots and lack of spatial information. It emphasizes that DVHs should be used along with visual analysis of dose distributions and dose-volume statistics when evaluating treatment plans.
Evolution of Intra-cavitary Brachytherapy

This document provides a history of brachytherapy and its evolution for treating cervical cancer. It discusses the early use of radium-222 and the development of intracavitary systems like Stockholm, Paris, and Manchester. Point A dose prescription and applicator design evolved over time. Later sources included cesium-137, iridium-192, and cobalt-60 used in remote afterloading. Overall, the document traces the development of brachytherapy techniques and technology for cervical cancer from the discovery of radiation to modern high dose rate treatments.
Brachytherapy permanent seed implant

Permanent brachytherapy, also called seed implantation, involves placing tiny radioactive seeds directly into the prostate tumor. The seeds remain permanently and give a continuous low dose of radiation over months to treat early stage prostate cancer. Common seeds used are iodine-125 or palladium-103. Precise pre-planning and ultrasound guidance ensures correct seed placement to maximize dose to the tumor while minimizing dose to nearby organs. Potential side effects include urinary symptoms and erectile dysfunction, though risks are lower than other treatments. Seed implantation provides high radiation directly to the tumor with less impact on healthy tissue compared to external beam radiation.
Linear Accelerator Acceptance, Commissioning and Annual QA

This document summarizes the expectations and key learnings from a linear accelerator acceptance, commissioning, and annual QA training that occurred from September to November 2008. The training covered:
1. Fundamental concepts of linear accelerators, beam production, safety features, and the acceptance testing process.
2. Techniques for collecting beam data needed for commissioning, including measurements and data definitions.
3. Procedures for linear accelerator QA and other treatment machine QA on an annual basis.
Key topics included the beamline components that produce photon and electron beams, characteristics of linear accelerator beams, the importance of acceptance testing and commissioning the machine properly, and techniques for annual QA tests.
Hsc 340 12 9

1. The document discusses various cancers of the gastrointestinal tract including esophageal, stomach, pancreatic, rectal, and anal cancers.
2. For each cancer, it describes the anatomy, routes of spread, common treatments including radiation therapy techniques and doses, and positioning and immobilization for radiation therapy.
3. It also discusses genitourinary cancers including bladder and prostate cancer as well as gynecological cancers focusing on uterine cervix cancer.
Hsc 340 11 18

This document discusses breast cancer, Hodgkin's lymphoma, and lung cancer. It provides details on:
- The most common types and treatments for breast cancer including surgery, radiation, and chemotherapy.
- The anatomy of the breast and common routes of cancer spread.
- Positioning and immobilization techniques for treating breast cancer with radiation.
- Common treatment techniques for breast cancer including tangents, boosts, and newer techniques like IGRT.
- Hodgkin's lymphoma presentation, staging, and common treatment approaches including radiation alone or with chemotherapy.
- Lung cancer risk factors, screening, and common treatment combinations of chemotherapy, surgery, and radiation.
- Anatomy of the lungs and considerations for
More Related Content
What's hot
TISSUE PHANTOM RATIO - THE PHOTON BEAM QUALITY INDEX

TPR(20,10) is the recommended photon beam quality index by IAEA TRS-398 for megavoltage clinical photons generated by linear accelerators. This presentation goes through the basics of Tissue Phantom Ratio (TPR).
Importance of Planning CT Simulation(3D) in Radiothrapy/Radiation oncology.

CT simulation is an important part of the radiotherapy planning process. It allows for 3D visualization of patient anatomy using CT scans. Various immobilization devices are used to accurately position the patient for treatment planning and delivery. The summary describes the key steps in CT simulation including patient setup using immobilization devices, obtaining CT images with appropriate parameters, and noting important details in the patient record for their specific diagnosis and treatment area. CT simulation provides critical 3D information to optimize radiotherapy treatment planning.
Exactrac 6D imaging overview

Radiosurgery combines stereotactic techniques and radiation beams to precisely deliver a high dose of radiation to tumors and lesions. The Exactrac system allows for frameless radiosurgery using infrared cameras and x-ray imaging to track internal anatomy and automatically position the patient for treatment without an invasive head frame. Treatment planning involves delineating the target and nearby organs at risk, specifying dose constraints, and optimizing the plan to conform the high dose region to the tumor while sparing surrounding healthy tissue.
Treatment plannings i kiran

Isodose curves depict absorbed dose distributions and variations in volume and planes. They join points of equal dose. Isodose charts show the variation in dose as a function of depth and transverse distance from the central beam axis. Factors like beam energy, field size, and distance affect isodose curve shape through penumbra and dose deposition. Multiple beams are often needed to adequately treat tumors while sparing surrounding tissues. Beam arrangements, weights, and modifiers must be optimized for each plan.
Electron beam therapy

Electron beam therapy uses accelerated electrons to treat superficial tumors. Electrons interact with matter through inelastic collisions that cause ionization and excitation, and elastic collisions that scatter the electrons. This gives electron beams a characteristically sharp dose drop-off beyond the tumor depth. Key applications of electron beams include treatment of skin cancers, chest wall irradiation for breast cancer, and boost doses to lymph nodes.
Beam modification 

This document discusses various beam modification devices used in radiation therapy. It describes the purpose of beam modification as altering the spatial distribution of radiation to better protect normal tissues and achieve uniform dose distribution. Common devices discussed include shielding blocks, wedges, compensators, and bolus. Shielding blocks are used to protect critical structures by blocking radiation to certain areas. Wedges are used to tilt isodose curves for improved dose conformity. Compensators are designed to even out irregular tissue surfaces. Bolus is placed on the skin to reduce the depth of maximum dose. The document provides details on the materials, design considerations, and clinical applications of these various beam modification tools.
Total skin electron irradiation 

Total skin electron irradiation ppt
Rupon Bhowmik
Dept of Medical physics & biomedical engineering,dhaka
Interstitial BT Principles

This document provides an overview of interstitial brachytherapy principles and concepts. It discusses the history and evolution of brachytherapy sources from radium to modern radioactive sources like iridium-192. Key concepts covered include dose rate calculations, implant systems like the Paris system, and factors that influence dose distribution from a radioactive source like distance, absorption and scattering. The document also describes temporary and permanent brachytherapy sources and different methods of source application including preloading, afterloading and remote afterloading.
Radioisotopes and dose rates used for brachytherapy

Radioisotopes and dose rates used for brachytherapy
This is the seminar about different radioisotopes used in brachytherapy beginning from radium to iradium and different dose rates, low dose rate, high dose rate used in brachytherapy. The significance of different dose rates and its radiobiology along with the clinical results.
Dosimetric Evaluation of High Energy Electron Beams Applied in Radiotherapy

Electron-beam therapy: is used to treat superficial tumors at a standard 100 cm source-to-surface distance (SSD). Characteristics of electron beams from an Elekta PreciseTM linear accelerator are presented at a nominal SSD of 100 cm. However, certain clinical situations require the use of an extended SSD. The effects of extended source-to-surface distance (SSD) on the electron beam dose profiles were evaluated for various electron beam energies 6, 8, 10,12 and 15 MeV and the accuracy of various output correction methods was analyzed on an Elekta PreciseTM linear accelerator using a radiation field analyzer (RFA). Effective SSDs was evaluated for field sizes ranging from 6×6, 10×10, 14×14 and 20×20 cm2 for various energies.
Aim of the work
1.Investigate the physical properties of electron beams
at different beam energies.
2.Evaluate the accuracy of dose calculated by
Treatment Planning System (TPS) and measured for
different field configurations.
Beam Directed Radiotherapy - methods and principles

Beam directed radiotherapy aims to deliver a homogenous tumor dose while minimizing radiation to normal tissues. It involves careful patient positioning, immobilization, tumor localization, field selection, dose calculations, and verification. Key steps include using positioning aids and molds to reproducibly position the patient, imaging such as CT to delineate the tumor volume, contouring to define external body outlines, and dose calculations and verification to ensure accurate delivery.
Motion management in Radiation Oncology - 2020

This document discusses various sources of uncertainty and errors in radiation therapy delivery due to patient and target motion. It describes advances in imaging guidance and motion management techniques like 4D imaging, respiratory gating, abdominal compression, and deep inspiration breath hold to minimize the effects of respiratory motion. Real-time tracking methods like RPM and ExacTrac systems are highlighted which allow continuous monitoring of tumor position throughout treatment. Managing respiratory motion remains an important area of focus to ensure accurate radiation delivery.
Isodose curves RADIATION ONCOLOGY

1. Isodose curves represent the dose distribution from radiation beams and are lines connecting points of equal percentage depth dose. They are used to depict the volumetric and planar variations in absorbed dose.
2. The parameters that affect the shape of isodose curves include beam quality, source size, SSD, SDD, field size, and beam modifiers like wedges and flattening filters. Lower beam energy results in greater lateral scatter and more bulging curves.
3. Multiple radiation fields can be combined using appropriate beam weights, sizes, angles and modifiers to deliver a more uniform dose to the tumor while sparing surrounding tissues. Parameters like setup accuracy and plan practicality are also considered.
linac QA.pptx

This document discusses quality assurance parameters and test frequencies for medical linear accelerators. It outlines electrical, mechanical, and dosimetry QA parameters that are tested daily, weekly, monthly, and yearly. Daily tests check parameters that could affect patient positioning, radiation field definition, output constancy, and safety. Weekly tests add checks for beam congruence, flatness, and symmetry. Monthly tests expand to all mechanical and electrical components. Annual tests involve re-calibration and more stringent tolerance levels to establish new baseline values. Tests ensure spatial and dosimetric accuracy within clinically acceptable limits.
Electron Beam Therapy

Updates on Electron Beam Therapy
I) Introduction
II) Central Axis Depth dose distribution
III) Dosimetric parametrics of electron beam
IV) Clinical Considerations of Electron beam therapy
Helical Tomotherapy

The document discusses helical tomotherapy, a form of radiation therapy that uses a rotating x-ray beam. It summarizes a study of 150 patients treated with tomotherapy between 2006-2007 for reasons such as complex tumor geometry or need for image guidance. Setup corrections were often needed based on pretreatment MV CT scans. Treatment times were typically under 25 minutes with minimal increases over time. Tomotherapy allows conformal dose distributions and image-guided radiation for difficult cases near critical organs.
Dose volume histogram

This document discusses dose-volume histograms (DVHs) which are used to analyze and compare radiation dose distributions in radiotherapy treatment planning. It describes how DVHs are generated by counting the number of voxels receiving different dose levels. DVHs can be displayed cumulatively or differentially and show the volume of structures receiving particular doses. The document outlines some limitations of DVHs including their insensitivity to small hot or cold spots and lack of spatial information. It emphasizes that DVHs should be used along with visual analysis of dose distributions and dose-volume statistics when evaluating treatment plans.
Evolution of Intra-cavitary Brachytherapy

This document provides a history of brachytherapy and its evolution for treating cervical cancer. It discusses the early use of radium-222 and the development of intracavitary systems like Stockholm, Paris, and Manchester. Point A dose prescription and applicator design evolved over time. Later sources included cesium-137, iridium-192, and cobalt-60 used in remote afterloading. Overall, the document traces the development of brachytherapy techniques and technology for cervical cancer from the discovery of radiation to modern high dose rate treatments.
Brachytherapy permanent seed implant

Permanent brachytherapy, also called seed implantation, involves placing tiny radioactive seeds directly into the prostate tumor. The seeds remain permanently and give a continuous low dose of radiation over months to treat early stage prostate cancer. Common seeds used are iodine-125 or palladium-103. Precise pre-planning and ultrasound guidance ensures correct seed placement to maximize dose to the tumor while minimizing dose to nearby organs. Potential side effects include urinary symptoms and erectile dysfunction, though risks are lower than other treatments. Seed implantation provides high radiation directly to the tumor with less impact on healthy tissue compared to external beam radiation.
Linear Accelerator Acceptance, Commissioning and Annual QA

This document summarizes the expectations and key learnings from a linear accelerator acceptance, commissioning, and annual QA training that occurred from September to November 2008. The training covered:
1. Fundamental concepts of linear accelerators, beam production, safety features, and the acceptance testing process.
2. Techniques for collecting beam data needed for commissioning, including measurements and data definitions.
3. Procedures for linear accelerator QA and other treatment machine QA on an annual basis.
Key topics included the beamline components that produce photon and electron beams, characteristics of linear accelerator beams, the importance of acceptance testing and commissioning the machine properly, and techniques for annual QA tests.
What's hot (20)
TISSUE PHANTOM RATIO - THE PHOTON BEAM QUALITY INDEX

TISSUE PHANTOM RATIO - THE PHOTON BEAM QUALITY INDEX
Importance of Planning CT Simulation(3D) in Radiothrapy/Radiation oncology.

Importance of Planning CT Simulation(3D) in Radiothrapy/Radiation oncology.
Radioisotopes and dose rates used for brachytherapy

Radioisotopes and dose rates used for brachytherapy
Dosimetric Evaluation of High Energy Electron Beams Applied in Radiotherapy

Dosimetric Evaluation of High Energy Electron Beams Applied in Radiotherapy
Beam Directed Radiotherapy - methods and principles

Beam Directed Radiotherapy - methods and principles
Linear Accelerator Acceptance, Commissioning and Annual QA

Linear Accelerator Acceptance, Commissioning and Annual QA
More from CSULB
Hsc 340 12 9

1. The document discusses various cancers of the gastrointestinal tract including esophageal, stomach, pancreatic, rectal, and anal cancers.
2. For each cancer, it describes the anatomy, routes of spread, common treatments including radiation therapy techniques and doses, and positioning and immobilization for radiation therapy.
3. It also discusses genitourinary cancers including bladder and prostate cancer as well as gynecological cancers focusing on uterine cervix cancer.
Hsc 340 11 18

This document discusses breast cancer, Hodgkin's lymphoma, and lung cancer. It provides details on:
- The most common types and treatments for breast cancer including surgery, radiation, and chemotherapy.
- The anatomy of the breast and common routes of cancer spread.
- Positioning and immobilization techniques for treating breast cancer with radiation.
- Common treatment techniques for breast cancer including tangents, boosts, and newer techniques like IGRT.
- Hodgkin's lymphoma presentation, staging, and common treatment approaches including radiation alone or with chemotherapy.
- Lung cancer risk factors, screening, and common treatment combinations of chemotherapy, surgery, and radiation.
- Anatomy of the lungs and considerations for
Hsc 340 10 28

This document discusses key concepts and calculations for radiation treatment planning including:
1) Concepts such as the treatment planning team, MU's, prescription, treatment time vs MU's, dose, depth, field size, and scatter.
2) Calculations for inverse square law, equivalent squares, tissue absorption factors like PDD and TAR, and SSD and SAD calculations.
3) Equations for determining dose rate modifiers, SSD, SAD, gap calculations between treatment fields.
Hsc 340 10 14

The document discusses various topics related to radiation therapy treatment planning including:
1. Photon and electron dose distributions, isodose distributions, beam profiles, corrections for obliquity and tissue heterogeneity.
2. Essentials of treatment planning including goals of conformal therapy to deliver 100% dose to tumor and 0% to critical structures, and use of 3D imaging and planning.
3. Algorithms for dose calculation including data-driven, model-driven, and factors for evaluation such as calculation accuracy and scatter integration.
Hsc 340 9 30

The document outlines standard treatment procedures for radiation therapy, including preparing the patient and treatment room, positioning the patient accurately, delivering the prescribed radiation dose using various beam shaping and modifying devices, and thoroughly documenting the treatment plan and each fraction delivered for quality assurance and record keeping. Proper patient identification, consent, dosimetry planning, beam positioning, monitoring, and documentation of any changes are emphasized.
Hsc 340 9 23

This document discusses electronic medical records (EMR) and their use in radiation oncology. It covers topics such as using EMR to consolidate and document patient healthcare information, the need for EMR in radiation oncology, computerized workflows and input methods, connectivity standards, information systems, data compilation for decision making and cancer registries, and considerations for implementing EMR such as security, privacy, and continuing education.
Hsc 340 9 16

The document summarizes the key steps in conventional and CT simulation procedures for radiation therapy treatment planning. These include diagnosis and staging of the cancer, therapeutic decisions, patient simulation using fluoroscopy or CT scanning for positioning and immobilization, treatment planning to identify target volumes and organs at risk, treatment delivery and monitoring, and patient follow-up. CT simulation allows for better visualization of anatomy and automatic contouring compared to conventional simulation. Both methods require accurate documentation of the simulation process.
Hsc 340 9 16

The document summarizes the key steps in conventional and CT simulation procedures for radiation therapy treatment planning. These include diagnosis and staging of the cancer, therapeutic decisions, patient simulation using fluoroscopy or CT scanning for positioning and immobilization, treatment planning to identify target volumes and organs at risk, treatment delivery and monitoring, and patient follow-up. CT simulation allows for better visualization of anatomy and automatic contouring compared to conventional simulation. Both methods require accurate documentation of the simulation process.
Hsc 340 9 9

The document provides a brief history of radiation therapy and x-rays, including their discovery in the late 19th century, and developments in equipment over time. It discusses early radiation therapy methods like orthovoltage and kilovoltage treatments. It also summarizes linear accelerators and how they improved upon older cobalt-60 and betatron technology to allow higher energy photon beams for treating deeper tumors. Simulation equipment is covered, comparing conventional versus CT-based simulation and how various imaging modalities can aid treatment planning.
Hsc 340

Cancer is caused by abnormal cell growth and proliferation due to environmental, genetic, and infectious factors. Tumors are classified as benign or malignant, with malignant tumors able to metastasize and invade other tissues. Cancer is detected through screening exams, tests, and imaging and is staged based on tumor size, lymph node involvement, and metastasis. Treatment may include surgery, chemotherapy, radiation therapy, and immunotherapy. Cancer spreads primarily via the lymphatic system and bloodstream, with patterns varying by cancer type. A patient's prognosis depends on factors like grade, stage, and tumor characteristics.
More from CSULB (10)
Ssd calculations
- 1. SSD Calculations • Patient surface at 100cm – (80cm for Co-60) – Usually a single beam – Most simple of all calculations – Most likely to be called upon to do 100 cm Dose to a point at depth Depth = d cm Source Patient Surface
- 2. The SSD Equation • MU Setting = Prescribed Dose . RDR x ISCF x Sc x Sp x (PDD/100) x Other Factors RDR = reference dose rate usually 1 cGy/MU (cGy/min for Co-60) ISCF = inverse square correction factor Sc = collimator scatter factor Sp = phantom scatter factor PDD = percent depth dose Other factors = trays, wedges, etc…
- 3. Case 1: 180 cGy to Dmax, 10x10 Open Field • MU Setting = Prescribed Dose . RDR x ISCF x Sc x Sp x (PDD/100) x Other Factors RDR = reference dose rate usually cGy/MU (cGy/min for Co-60) ISCF = inverse square correction factor Sc = collimator scatter factor Sp = phantom scatter factor PDD = percent depth dose Other factors = trays, wedges, etc… RDR = 1 cGy/MU ISCF = N/A = 1.000 Sc = 1.000 Sp = 1.000 PDD = 100% Other factors = N/A = 1.000 • MU Setting = 180 . 1 x 1.000 x 1.000 x 1.000 x (100/100) x 1.000 = 180 MU 100 cm Depth = dmax = 1.5 cm 10x10 Field Size
- 4. Case 2: 180 cGy to d = 5 cm, 10x10 Open Field • MU Setting = Prescribed Dose . RDR x ISCF x Sc x Sp x (PDD/100) x Other Factors RDR = reference dose rate usually cGy/MU (cGy/min for Co-60) ISCF = inverse square correction factor Sc = collimator scatter factor Sp = phantom scatter factor PDD = percent depth dose Other factors = trays, wedges, etc… RDR = 1 cGy/MU ISCF = N/A = 1.000 Sc = 1.000 Sp = 1.000 PDD = 87.1% Other factors = N/A = 1.000 • MU Setting = 180 . 1 x 1.000 x 1.000 x 1.000 x (87.1/100) x 1.000 = 207 MU 100 cm Depth = 5 cm 10x10 Field Size
- 5. Case 3: 180 cGy to d = 5 cm, 10x20 Open Field • MU Setting = Prescribed Dose . RDR x ISCF x Sc x Sp x (PDD/100) x Other Factors RDR = reference dose rate usually cGy/MU (cGy/min for Co-60) ISCF = inverse square correction factor Sc = collimator scatter factor Sp = phantom scatter factor PDD = percent depth dose Other factors = trays, wedges, etc… RDR = 1 cGy/MU ISCF = N/A = 1.000 Sc = 1.013 (Based Upon 13x13 equivalent square) Sp = 1.008 (Based Upon 13x13 equivalent square) PDD = 87.7% (Based Upon 13x13 equivalent square) Other factors = N/A = 1.000 • MU Setting = 180 . 1 x 1.000 x 1.013 x 1.008 x (87.7/100) x 1.000 = 201 MU 100 cm 10x20 Field Size Depth = 5 cm
- 6. Case 4: 180 cGy to d = 5 cm, 10x20, 20% blocked field • MU Setting = Prescribed Dose . RDR x ISCF x Sc x Sp x (PDD/100) x Other Factors RDR = reference dose rate usually cGy/MU (cGy/min for Co-60) ISCF = inverse square correction factor Sc = collimator scatter factor Sp = phantom scatter factor PDD = percent depth dose Other factors = trays, wedges, etc… RDR = 1 cGy/MU ISCF = N/A = 1.000 Sc = 1.013 (Based Upon 13x13 equivalent square) Sp = 1.005 (Based Upon 11.7x11.7 effective square) PDD = 87.4% (Based Upon 11.7x11.7 effective square) Other factors = 0.970 (a blocking tray transmission factor) • MU Setting = 180 . 1 x 1.000 x 1.013 x 1.005 x (87.4/100) x 0.970 = 208 MU 100 cm 10x20 Field Size Depth = 5 cm
- 7. Case 5: 180 cGy to d = 5 cm, 10x20, 20% blocked field, SSD = 110 cm* *Ignoring Mayneord Factor • MU Setting = Prescribed Dose . RDR x ISCF x Sc x Sp x (PDD/100) x Other Factors RDR = reference dose rate usually cGy/MU (cGy/min for Co-60) ISCF = inverse square correction factor Sc = collimator scatter factor Sp = phantom scatter factor PDD = percent depth dose Other factors = trays, wedges, etc… RDR = 1 cGy/MU ISCF = (101.52 /111.52 ) = 0.828 Sc = 1.007 (Based Upon 11.8x11.8 equivalent square) Sp = 1.005 (Based Upon 11.7x11.7 effective square) PDD = 87.4% (Based Upon 11.7x11.7 effective square) Other factors = 0.970 (a blocking tray transmission factor) • MU Setting = 180 . 1 x 0.828 x 1.007 x 1.005 x (87.4/100) x 0.970 = 253 MU 110 cm 10x20 Field Size on the patient Depth = 5 cm 9.1x18.2 Field Size on the machine
- 8. Case 6: 180 cGy to d = 5 cm, 10x20, 20% blocked field, SSD = 110 cm* *Including Mayneord Factor • MU Setting = Prescribed Dose . RDR x ISCF x Sc x Sp x (PDD/100) x Other Factors RDR = reference dose rate usually cGy/MU (cGy/min for Co-60) ISCF = inverse square correction factor Sc = collimator scatter factor Sp = phantom scatter factor PDD = percent depth dose Other factors = trays, wedges, etc… RDR = 1 cGy/MU ISCF = (101.52 /111.52 ) = 0.828 Sc = 1.007 (Based Upon 11.8x11.8 equivalent square) Sp = 1.005 (Based Upon 11.7x11.7 effective square) PDD = 87.4% x (1052 )/(101.52 ) x (111.52 )/(1152 ) = 87.9% Other factors = 0.970 (a blocking tray transmission factor) • MU Setting = 180 . 1 x 0.828 x 1.007 x 1.005 x (87.9/100) x 0.970 = 252 MU 110 cm 10x20 Field Size on the patient Depth = 5 cm 9.1x18.2 Field Size on the machine
- 9. Case 7: Rx 180 cGy to d = 5cm, what is the dose to dmax? In an SDD setup, the doses inside the patient are related by the ratio of PDDs. Dose Dmax = 180 cGy x PDD(dmax) / PDD(d=5) = 180 x 100 / 87.1 = 206.7 cGy 100 cm Depth = 5 cm 10x10 Field Size dmax
- 10. Mayneord Factor