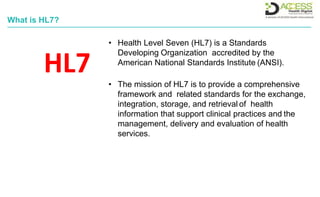
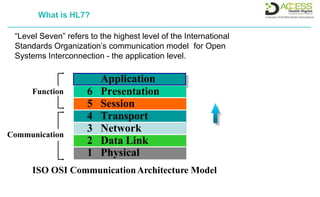
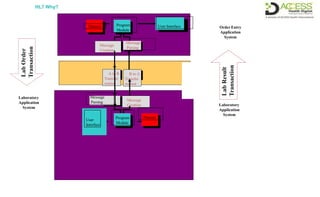
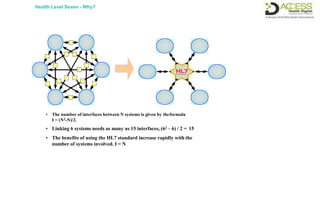
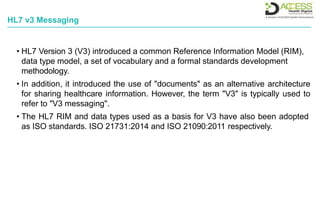
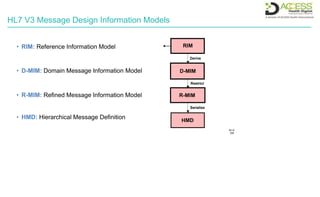
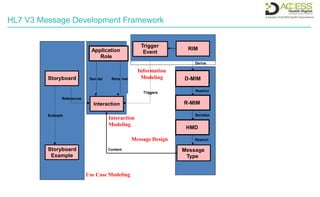
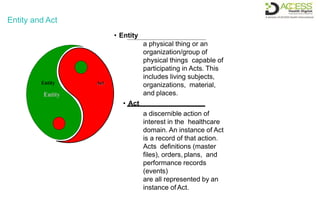
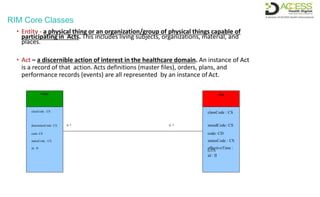
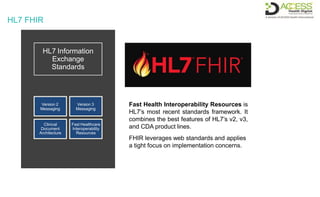
The document discusses HL7 and FHIR. It begins by explaining that HL7 is a standards development organization that provides a framework and standards for exchanging health information to support clinical practices and health services management. It then defines what "Level Seven" refers to in relation to the ISO communication model. The document also provides information on various HL7 product families, including FHIR, CDA, EHR functional model, SOA, and context management architecture. It concludes by summarizing HL7 Version 2 and Version 3 messaging standards.

![Abstract Message Specification
Guarant
or
Insurance
Insurance Additional
Info. Insurance Add'l
Info - Cert.
[ ] optional
Segment
ID
MSH
EVN
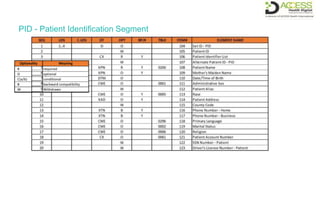
PID
[PD1]
[ { NK1
} ]
PV1
[ PV2 ]
…
[ { GT1
} ] [
{ IN1
[ IN2 ]
[ IN3 ]
}
]
…
Segment
Name Message
Header Event
Type
Patient Identification
Additional
Demographics
Next of Kin /Associated
Parties Patient Visit
Patient Visit - Additional
Info
. { } may repeat](https://image.slidesharecdn.com/hl7fhir-210525101412/85/Hl7-FHIR-7-320.jpg)


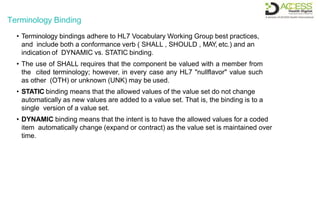


![Terminology Binding
• a hierarchical table that presents a
logical view of the content
• a UML diagram thatsummarizes
the content graphically
• a pseudo-XML syntax that
provides a visual sense of what
the end resource instances will
look like in XML
• a pseudo-JSON syntax that
provides a visual sense of what
the end resource instances will
look like in JSON
• a pseudo-Turtle syntax that
provides a visual sense of what
the end resource instances will
look like in Turtle
Specification Data Element
- identifier: ST
- type: CD
codeSystem.identifier: ST [0..1]
- codeValue: ST [0..1]
name: ST
- valueSet.identifier: ST [0..1]
- /codeSystemTerm.identifier: ST [0..1]
- /valueSetMemberIdentifier: ST [0..1]
Code System
- identifier: ST
- name:ST
- OID:Uid
Code System Term
- codeValue: ST
- codeSystem.identifier: ST
- /identifier: ST
- name: ST
Value Set Member
- codeValue: ST
- codeSystem.identifier: ST
- preferredName: ST [0..1]
- /identifier: ST
- valueSet.identifier: ST
- /codeSystemTerm.identifier: ST
Value Set
- identifier: ST
- name:ST
- OID:Uid
0..* 0..*
1
0..* -
0..1
0..*
0..1
0..*
0..1
Terminology Binding
0..*
0..* -
0..1](https://image.slidesharecdn.com/hl7fhir-210525101412/85/Hl7-FHIR-43-320.jpg)
