This presentation provides an overview of HIV and AIDS, including:
1. Definitions of HIV as the virus that causes AIDS and weakens the immune system, and AIDS as the final stage of HIV infection.
2. HIV-1 is the most common type worldwide and generally causes AIDS faster than HIV-2, which is mostly found in West Africa.
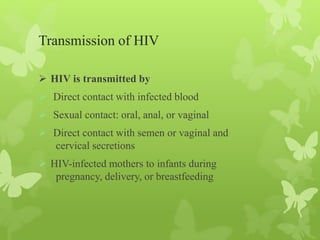
3. HIV is transmitted through bodily fluids and can be spread through unprotected sex, blood contact, or from mother to child during pregnancy or breastfeeding. Proper precautions can prevent transmission.
![Pathogenesis & Immunity
HIV infects helper T cells (CD4-positive cells) and kills them,
resulting in suppression of cell-mediated immunity. This predisposes
the host to various opportunistic infections and certain cancers such as
Kaposi’s sarcoma[1] and lymphoma. HIV does not directly cause these
tumors because HIV genes are not found in these cancer cells.
The initial infection of the genital tract occurs in dendritic cells that
line the mucosa (Langerhans’ cells), after which the local CD4-
positive helper T cells become infected. HIV is first found in the blood
4 to 11 days after infection.](https://image.slidesharecdn.com/hivinfection-200225160520/85/Hiv-infection-16-320.jpg)