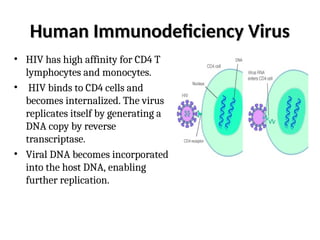
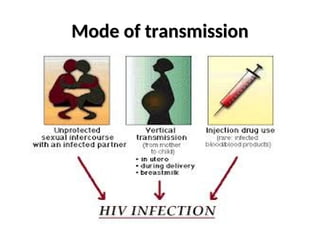
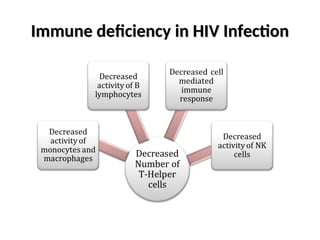
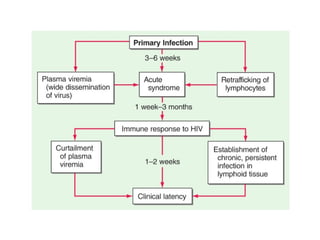
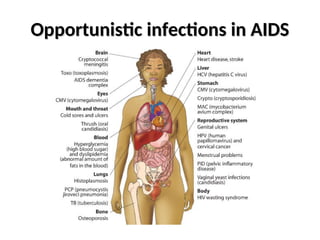
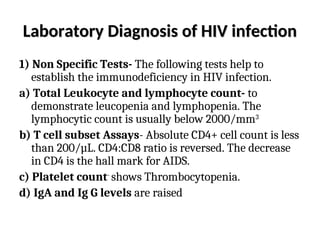
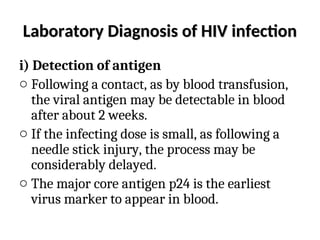
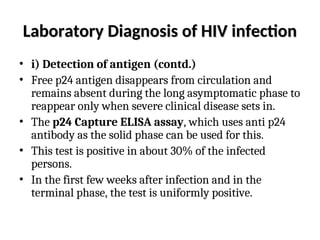
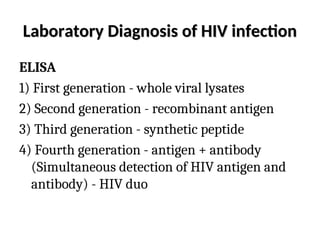
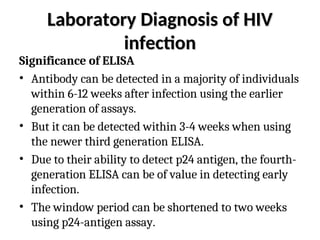
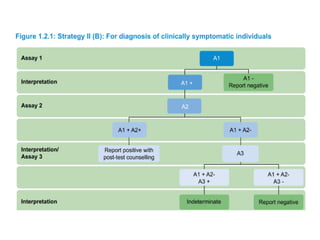
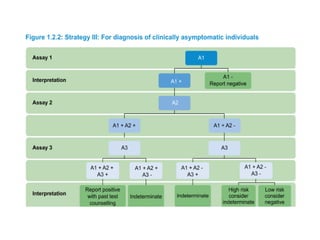
Acquired Immunodeficiency Syndrome (AIDS) is caused by the Human Immunodeficiency Virus (HIV) and leads to significant immunosuppression in affected individuals. HIV is primarily transmitted through sexual contact, blood transfusions, needle sharing, or from mother to child, and about 5-10% of individuals may not progress to AIDS for over 15 years, known as 'long-term survivors.' While screening for HIV is commonly done using ELISA and confirmed through Western blotting, there is currently no cure or vaccine available, and treatment aims only to manage disease progression.