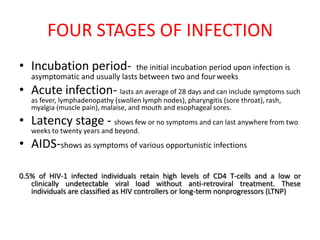
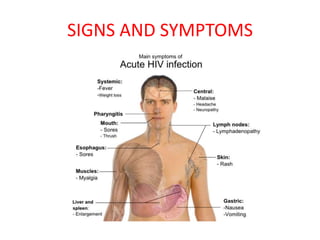
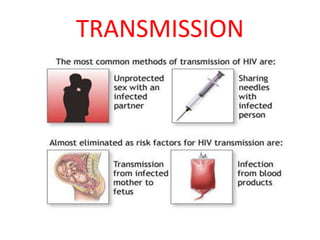
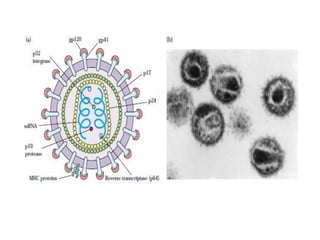
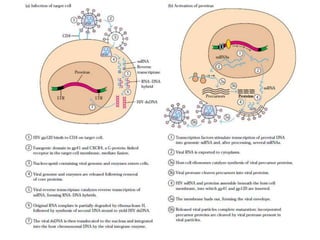
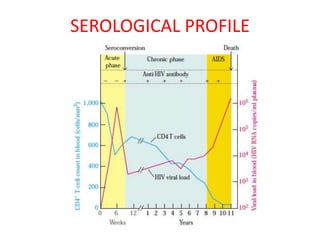
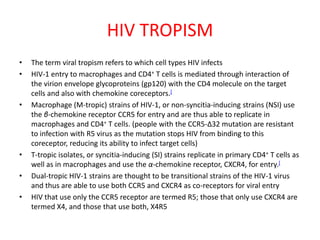
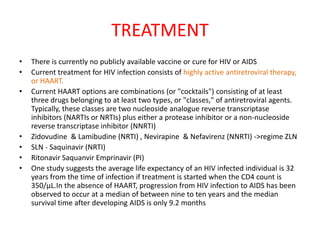
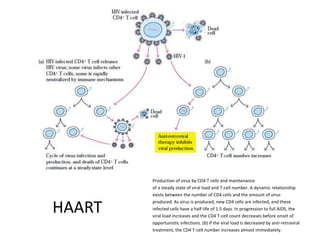
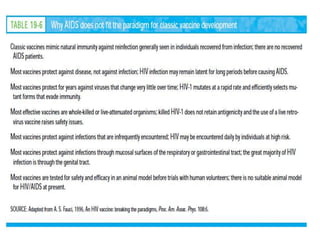
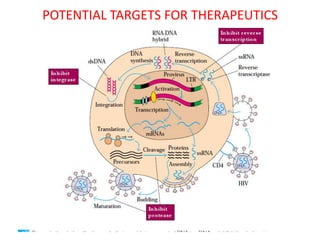
Secondary immunodeficiency results from exposure to agents and the most common form is AIDS caused by HIV. HIV is a lentivirus classified as HIV-1 or HIV-2. It has four stages: incubation, acute infection, latency and AIDS. Current treatment consists of combinations of at least three antiretroviral drugs from two classes. While treatment can suppress the virus and increase CD4 counts, there is no vaccine or cure for HIV/AIDS.