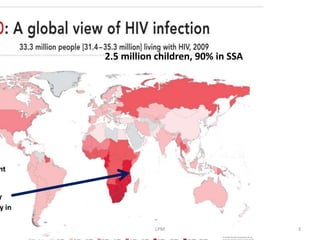
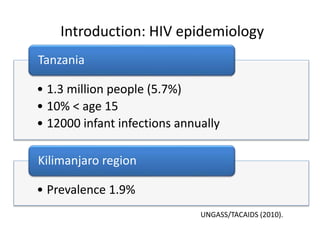
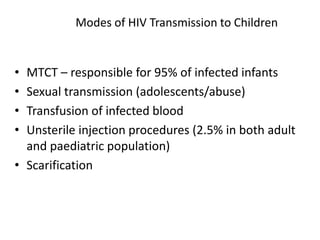
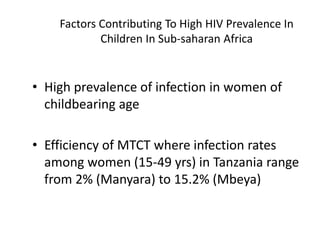
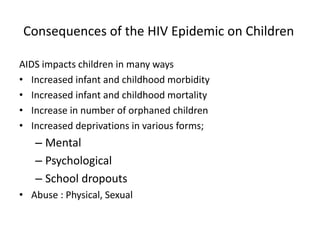
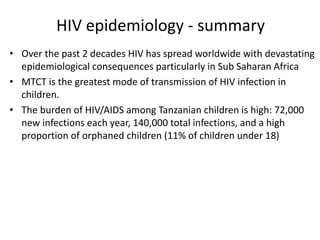
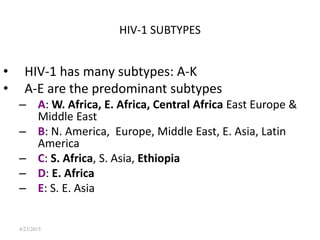
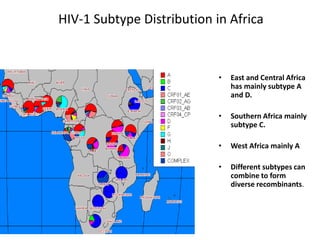
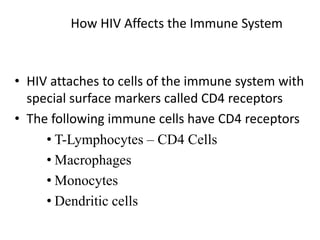
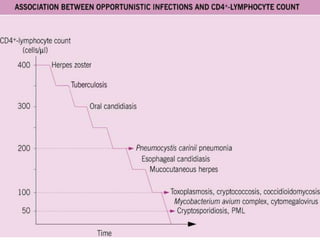
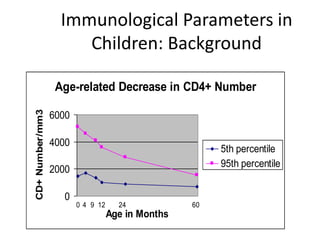
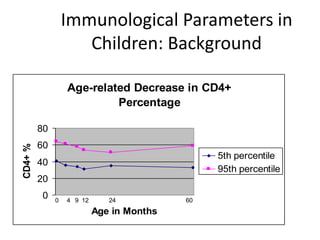
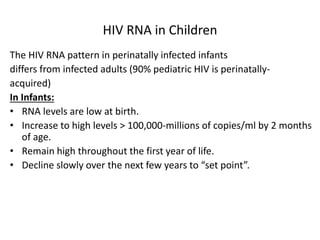
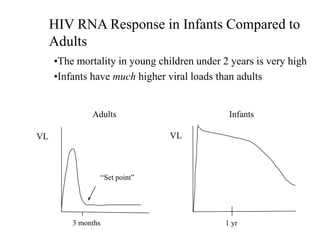
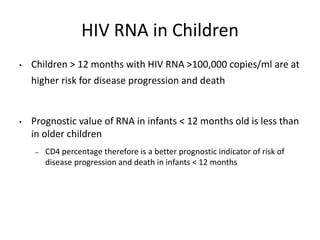
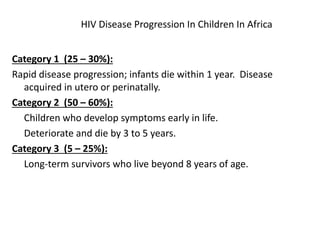
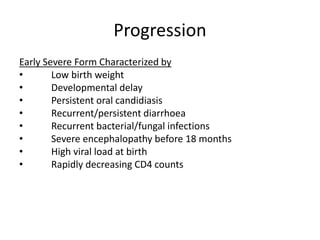
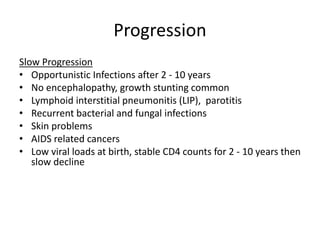
HIV infection in children is a major public health problem, especially in Sub-Saharan Africa. Over 2.5 million children are living with HIV globally, with over 95% of pediatric infections resulting from mother-to-child transmission. Factors like high HIV prevalence in women of childbearing age and subtype C's increased virulence have led to high rates of pediatric infection in Tanzania and SSA. HIV depletes CD4+ T cells, impairing immune function and leaving children susceptible to opportunistic infections. Disease progression varies but can be rapid, with mortality high in infants under 2 years old due to inability to control high viral loads.