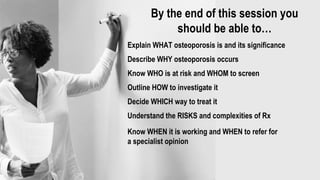
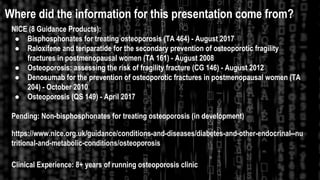
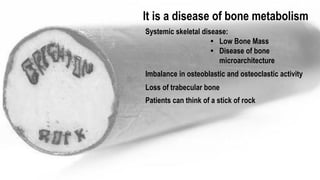
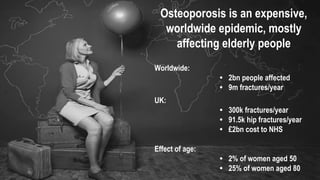
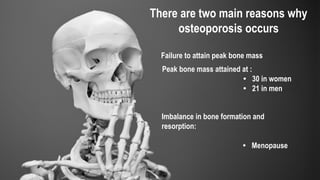
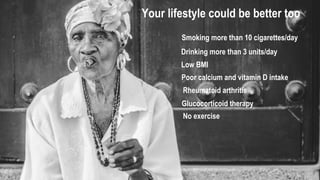
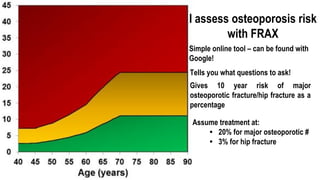
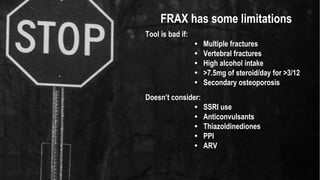
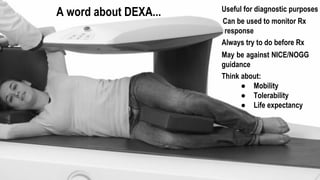
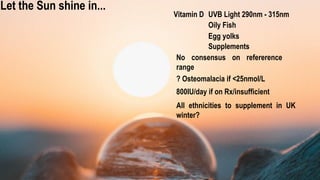
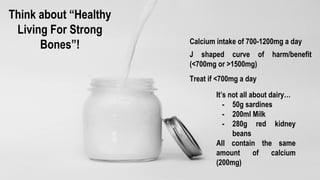
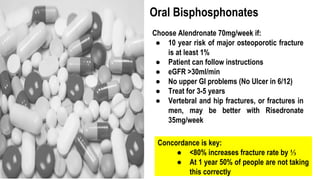
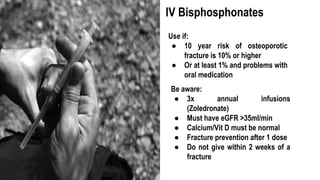
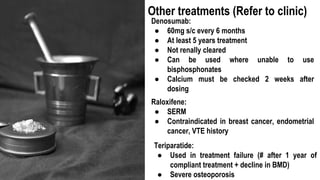
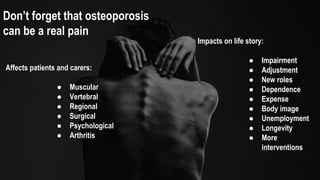
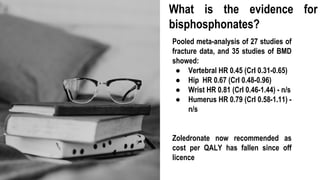
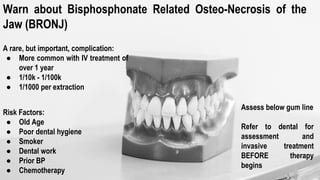
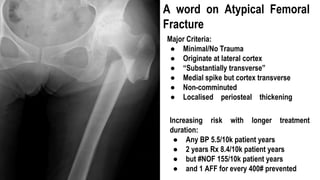
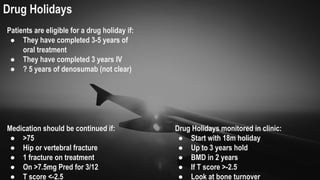
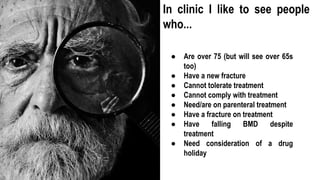
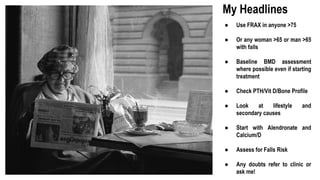
The document presents a comprehensive overview of osteoporosis, including its definition, risk factors, screening methods, treatment options, and management strategies. It highlights the significance of early detection and lifestyle modifications while emphasizing the need for appropriate medical interventions to prevent complications like fractures. The information is supported by clinical experience and guidelines from established medical organizations.