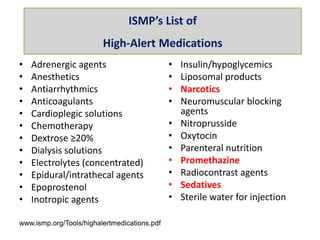
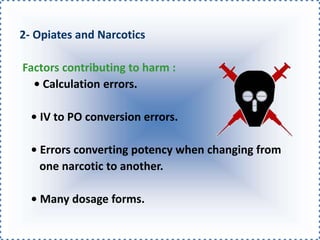
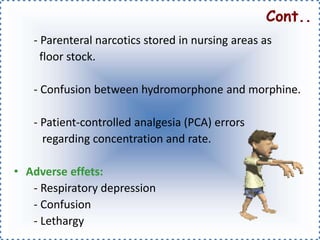
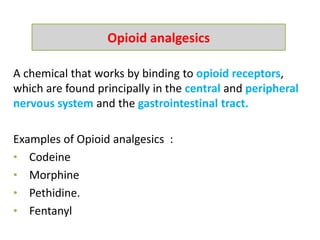
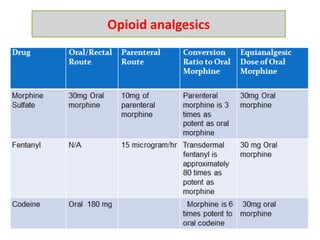
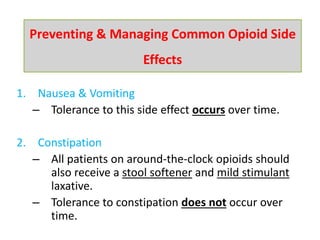
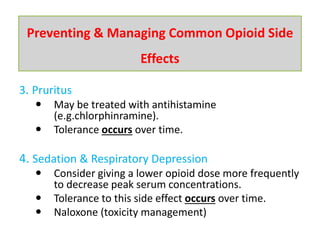
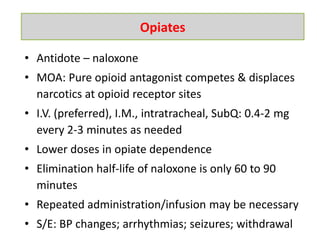
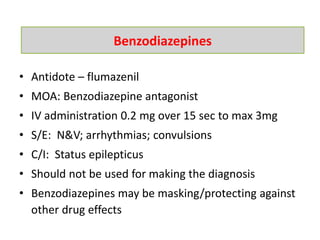
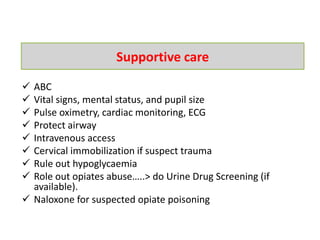
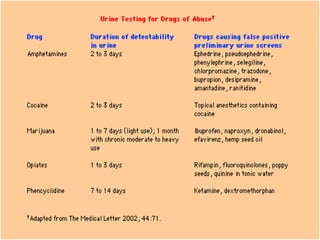
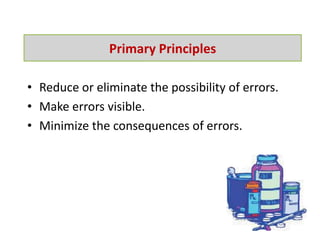
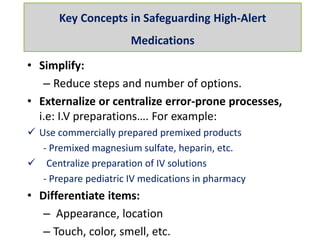
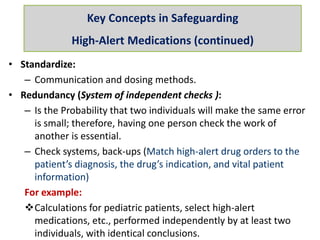
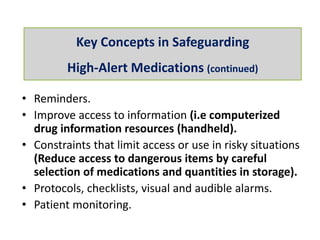
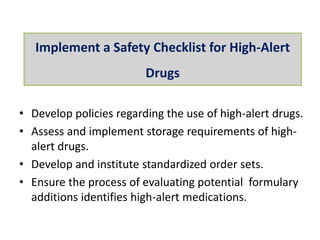
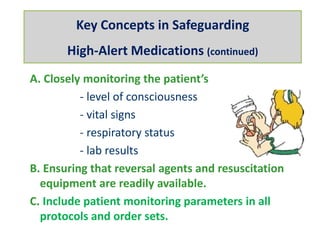
This presentation discusses high-alert medications, which are drugs that carry an increased risk of harming patients if used incorrectly. It identifies common classes of high-alert medications like opioids, insulin, and anticoagulants. Case scenarios are presented to demonstrate potential harms from improper use. Strategies are described for safely monitoring high-alert medications through standardization, redundancy checks, simplifying processes, and close patient monitoring.