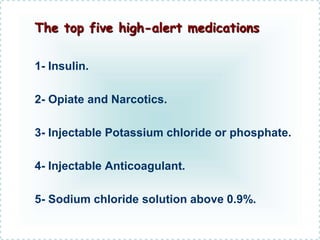
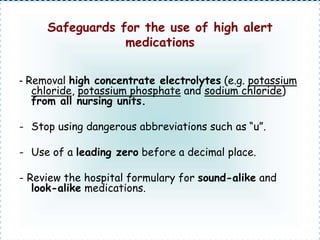
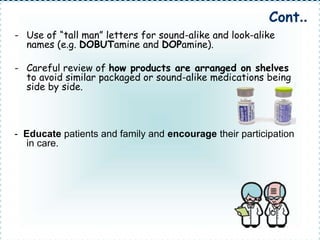
The document discusses the critical issue of medication errors in hospitals, focusing on high alert medications that pose significant risks to patients if used incorrectly. It identifies the top five high-alert medications and recommends strategies to reduce the risk of errors, such as removing high-concentration electrolytes from nursing units and educating patients. The presentation aims to implement better procedures in the hospital to enhance patient safety.