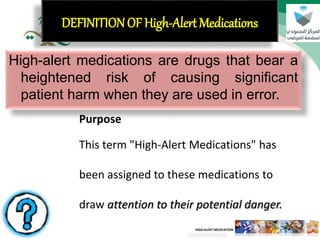
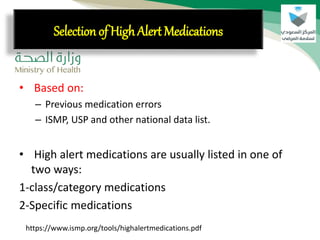
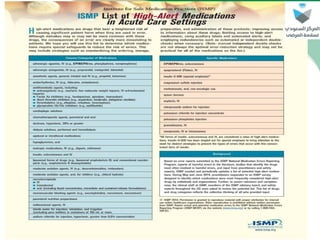
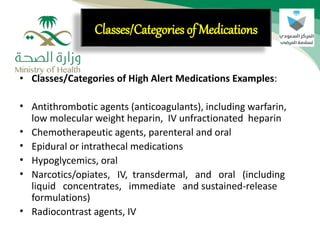
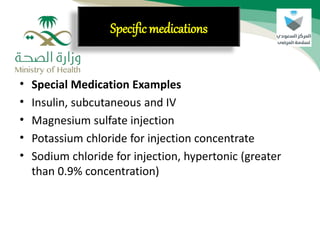
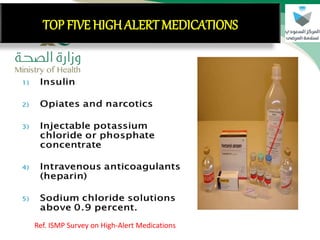
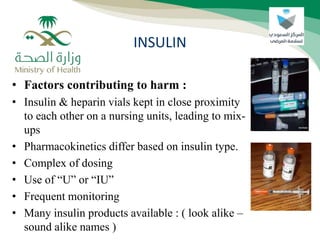
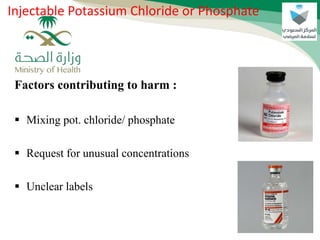
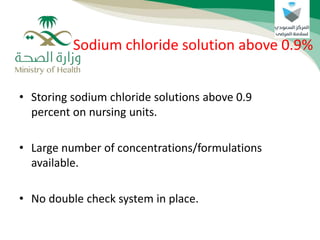
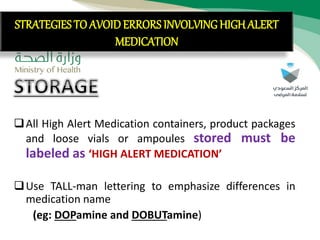
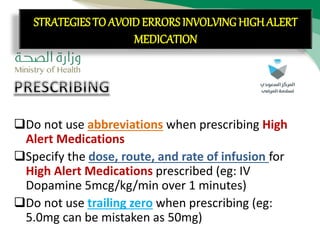
High-alert medications, which pose a significant risk of patient harm when used in error, include categories like anticoagulants and narcotics. Common risk factors leading to errors involve confusion between similar medications, incorrect administration methods, and unclear labeling. To minimize these risks, strategies such as proper labeling, independent verification of medication details, and comprehensive training for personnel handling these drugs are essential.