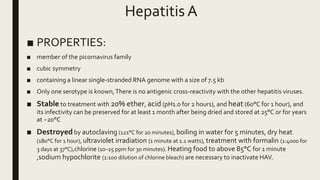
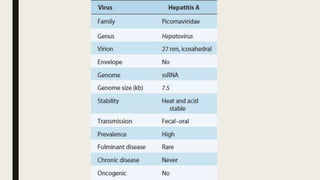
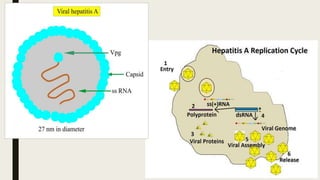
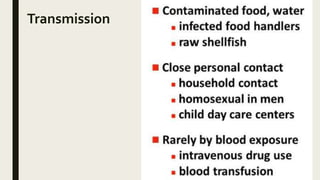
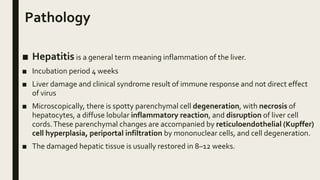
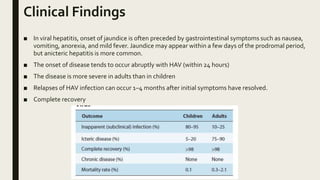
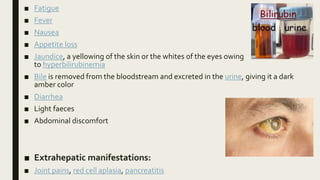
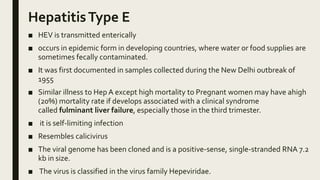
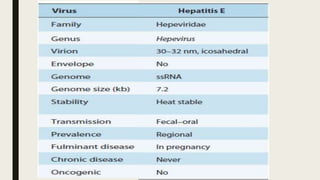
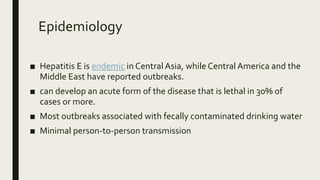
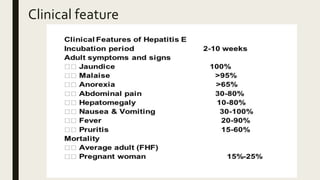
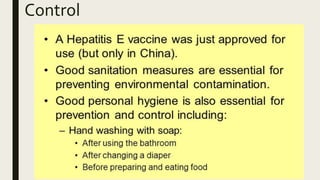
Hepatitis can be caused by several viruses and other factors. Hepatitis A virus (HAV) causes an acute form of hepatitis that is often self-limiting. HAV is transmitted through the fecal-oral route and spreads through contaminated food or water. It has an incubation period of 4 weeks and causes liver inflammation. Hepatitis E virus (HEV) also causes an acute form of hepatitis through contaminated food or water. While self-limiting in most patients, HEV infection during pregnancy can lead to fulminant liver failure and death, especially in the third trimester. Prevention efforts focus on handwashing and water treatment to prevent transmission.