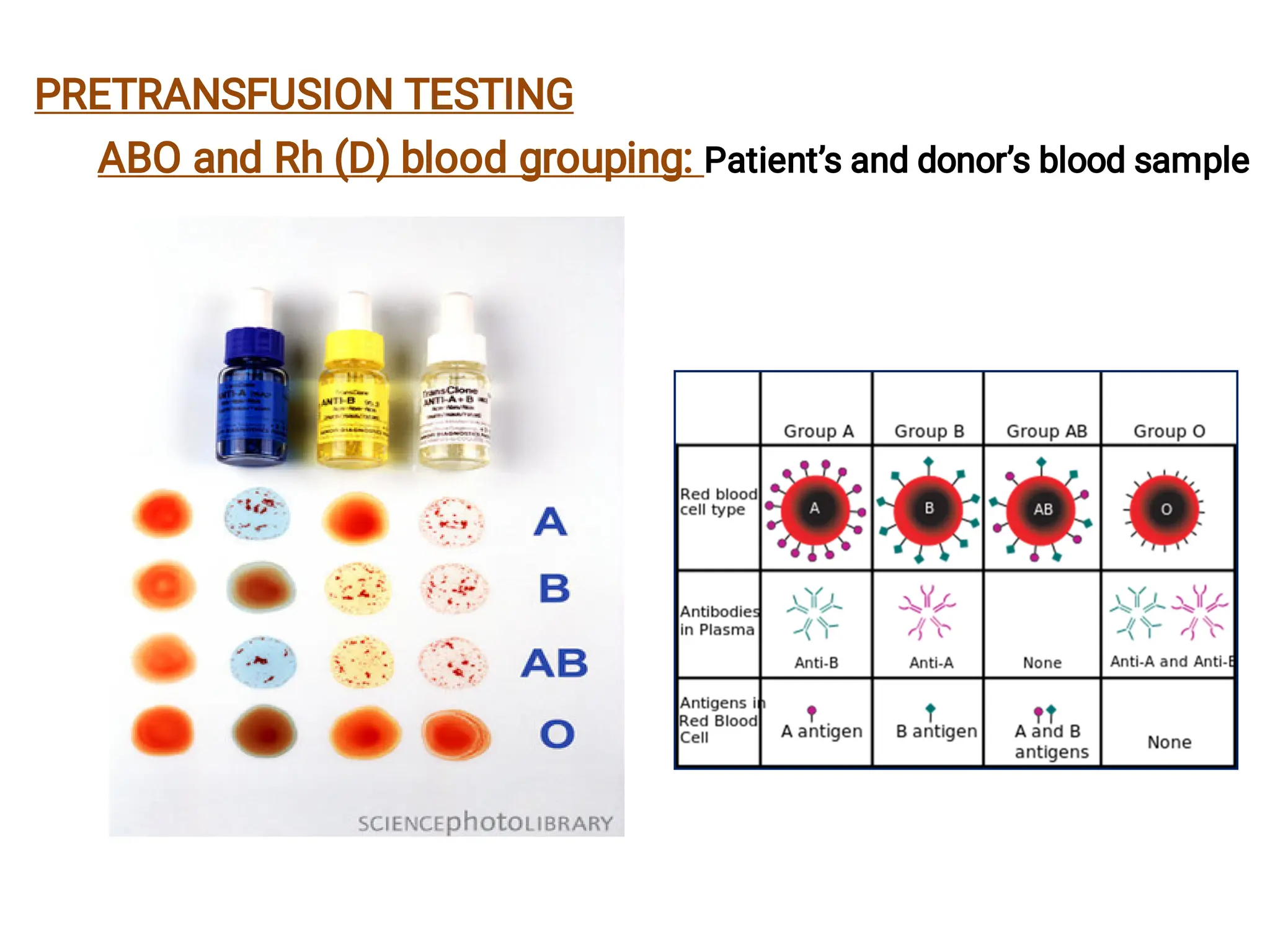
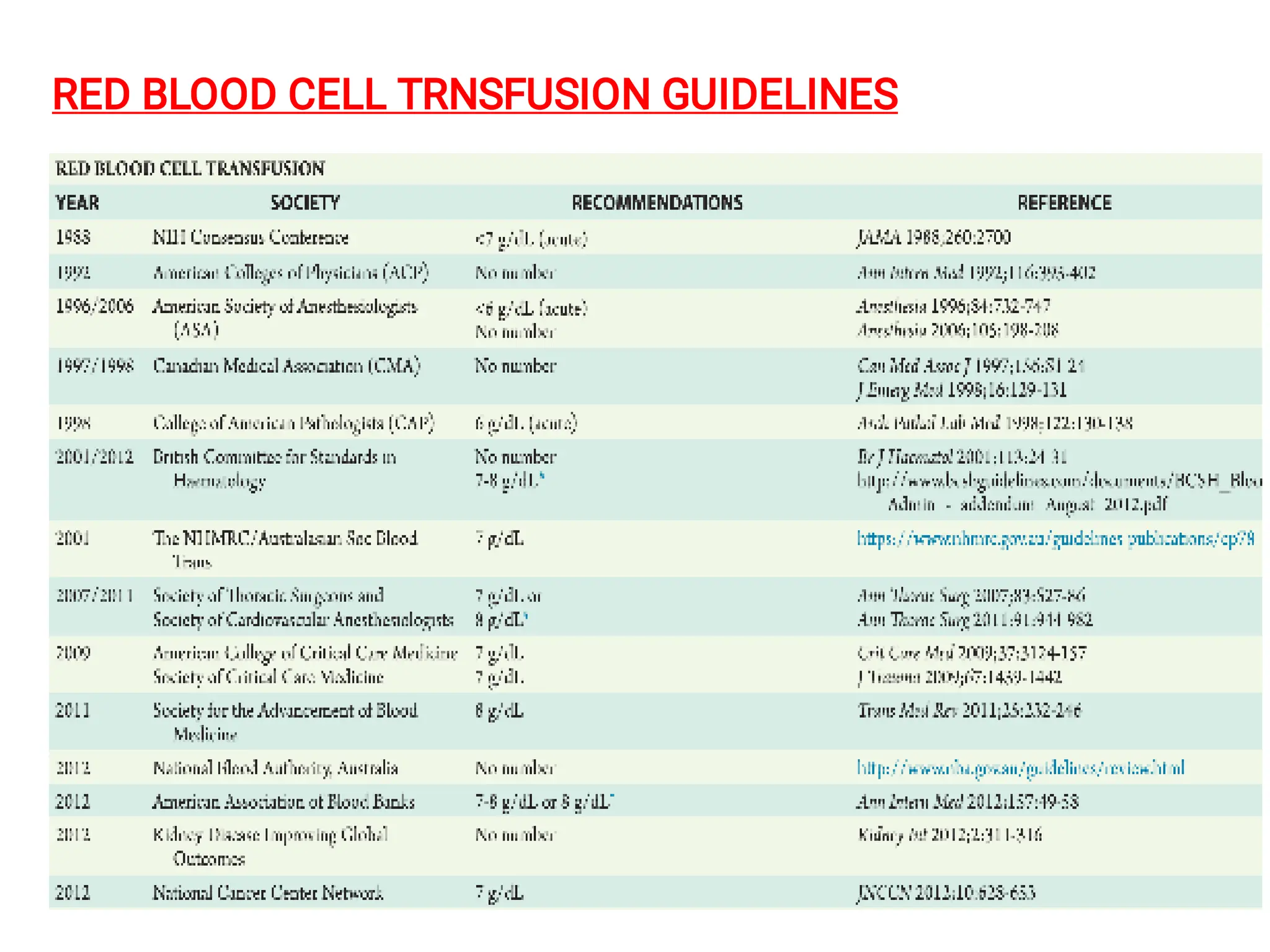
The document discusses blood transfusions and their potential reactions, focusing on blood group antigens, compatibility testing, and the various components of blood products like red blood cells, platelets, and plasma. It details risks associated with transfusions, including immune-mediated and non-immunologic reactions, and outlines treatment options for complications that may arise. Additionally, it emphasizes the importance of proper blood donor selection, testing, and storage conditions to enhance transfusion safety.