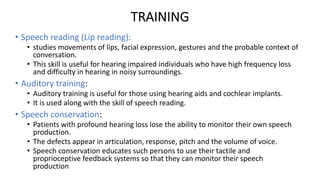
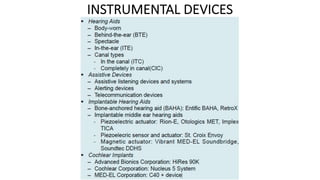
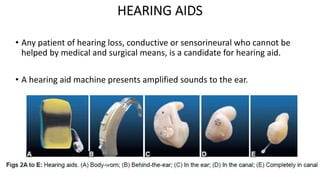
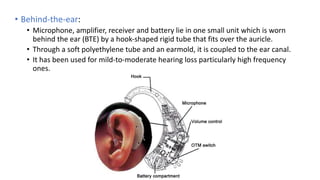
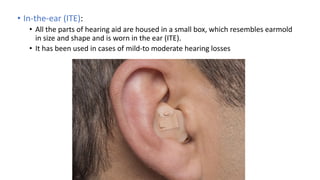
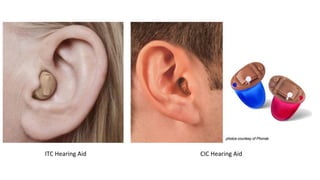
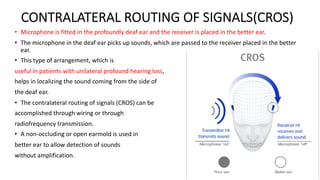
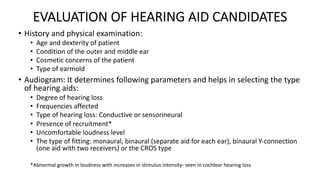
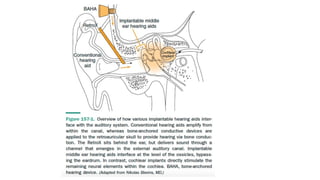
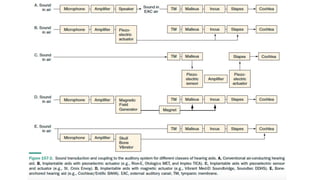
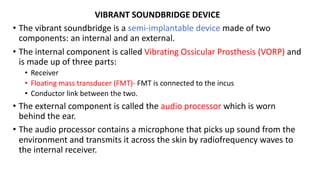
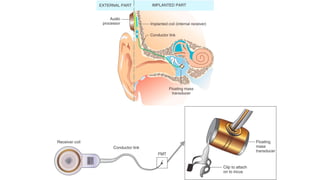
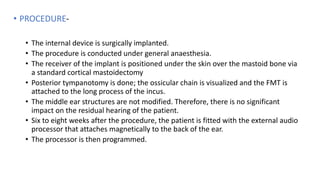
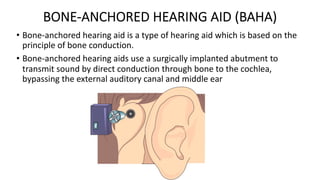
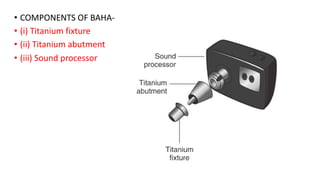
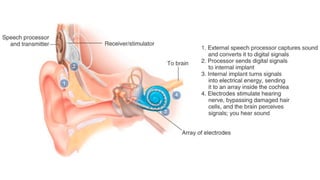
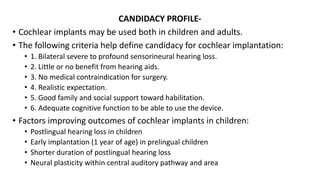
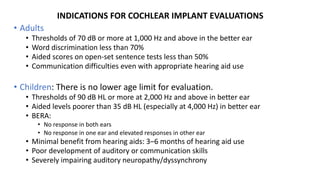
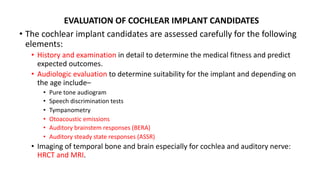
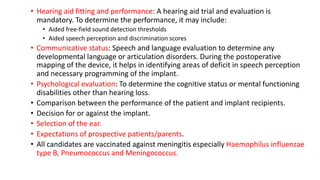
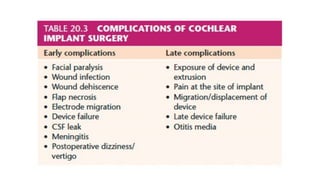
The document provides a comprehensive overview of auditory rehabilitation, including the use and types of hearing aids, cochlear implants, and their evaluation. It details various auditory training methods, components of hearing aids, their acoustic properties, as well as candidacy profiles and the procedure for implantable devices like bone-anchored hearing aids and middle ear implants. The information is aimed at understanding the various options available for individuals with hearing loss, including their advantages, indications, and complications.