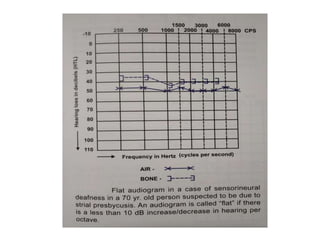
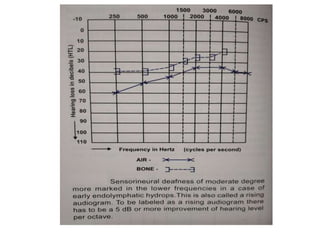
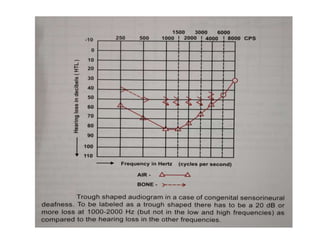
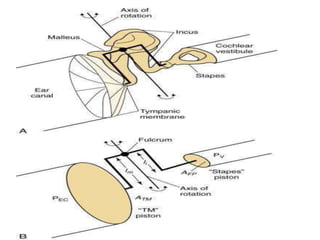
The document discusses audiometry, detailing sound waves, their propagation, and the physiology of human hearing. It explains the function of the ear, including sound collection, transformation through the middle ear, and the significance of pure tone audiometry in assessing hearing loss. Various conditions affecting hearing and tympanoplasty techniques are also explored, emphasizing the importance of restoring sound conduction mechanisms.



















































![% of Handicap
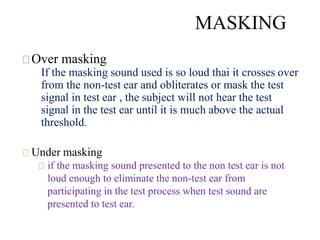
Formula for calculating % of handicap for unilateral
deafness –{ [( a+b+c+d)÷ 4 ]- 25} x 1.5%
where a,b,c and d are air conduction threshold at
500, 1000,2000, and 3000Hz respectively
Bilateral – [ (5x +y) ÷6 ]%
where x and y are the percentage of handicap for the
better and worse ear respectively](https://image.slidesharecdn.com/puretoneaudiometry-200229190658/85/Pure-Tone-Audiometry-73-320.jpg)