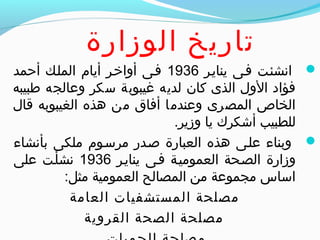
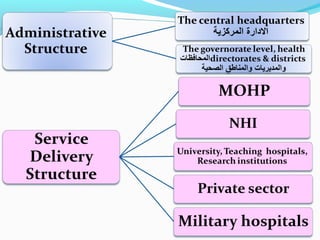
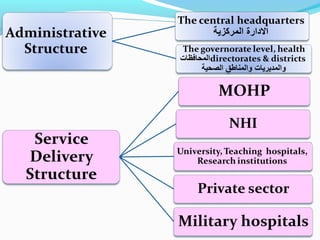
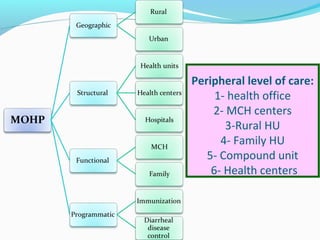
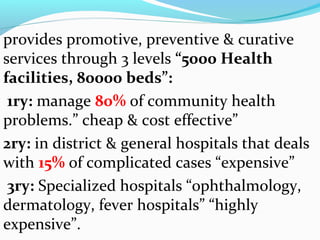
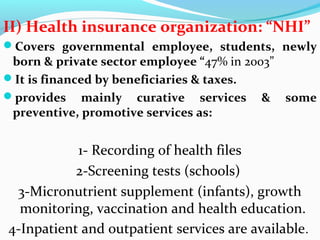
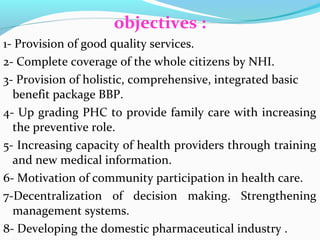
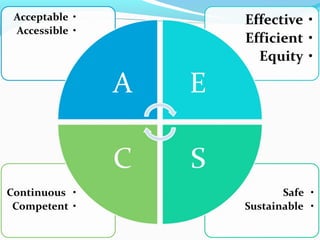
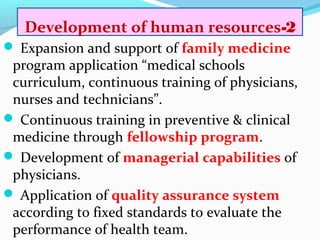
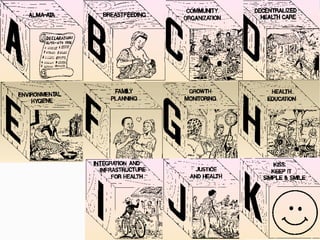
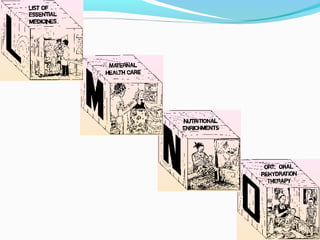
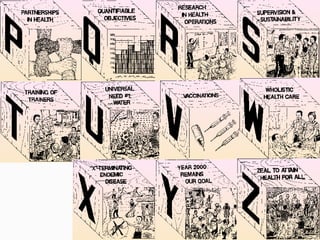
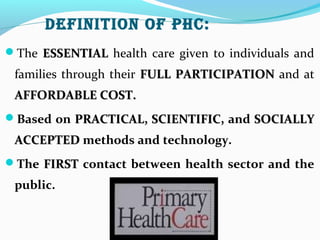
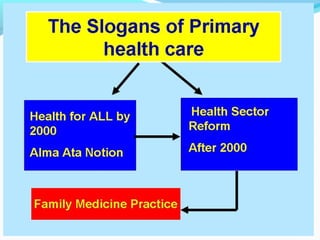
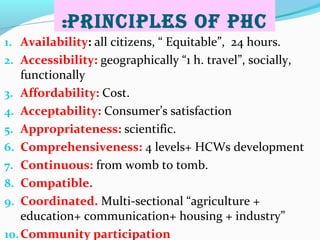
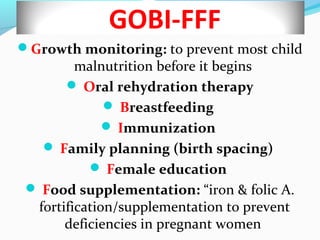
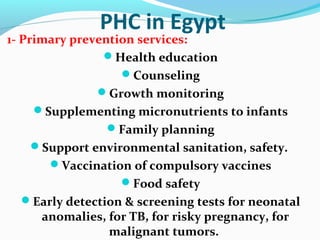
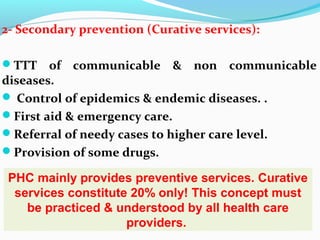
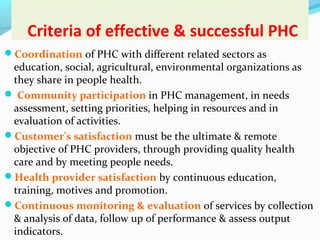
The document discusses health services and primary health care in Egypt. It provides background on the Ministry of Health and Population, which was established in 1936. It outlines Egypt's health system, which includes primary, secondary, and tertiary levels of care provided through public health units and hospitals. The document also discusses health insurance in Egypt, challenges in the health system, and strategic plans for health sector reform focusing on infrastructure development and improving human resources. It defines primary health care and reviews its principles, approaches like GOBI-FFF, essential services, and role in Egypt through primary health units. Criteria for effective primary health care include coordination, community participation, customer satisfaction, and monitoring and evaluation.