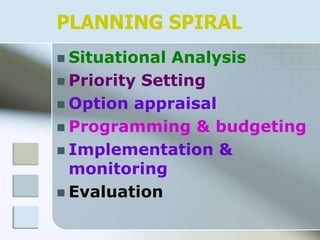
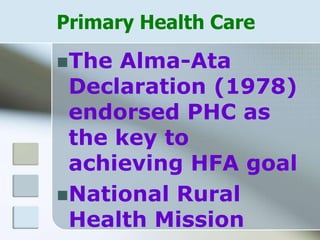
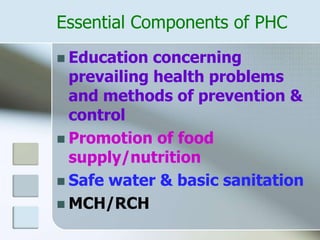
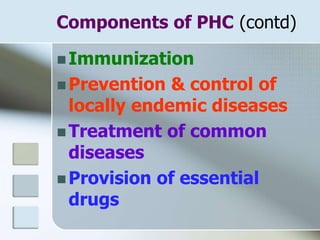
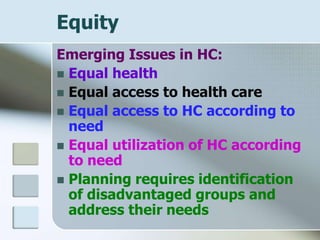
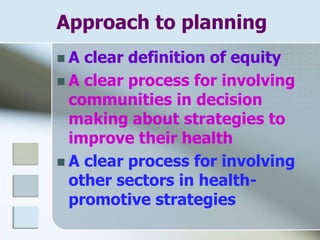
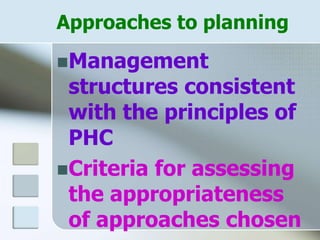
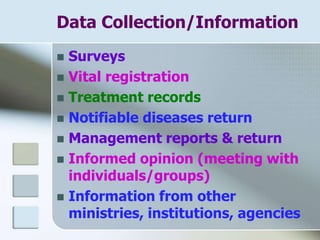
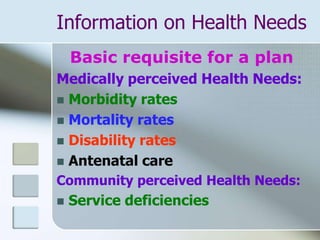
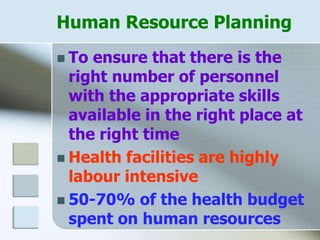
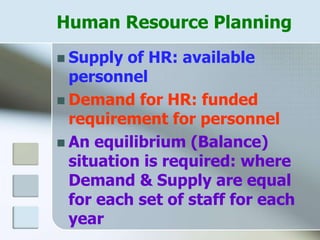
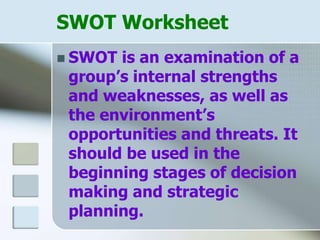
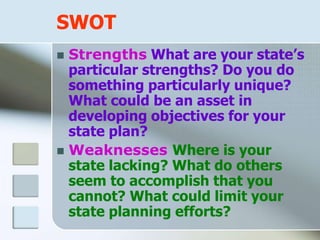
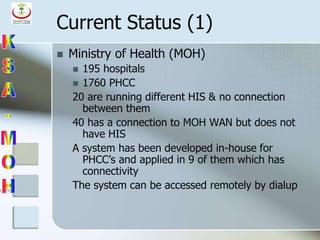
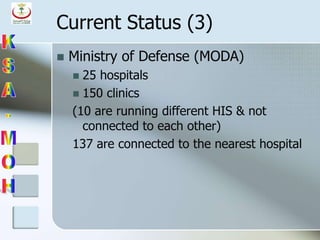
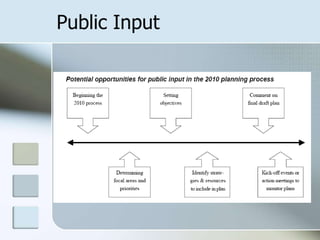
The document discusses health planning and the responsibilities of doctors. It notes the pressures of knowledge explosion, technological advances, and information sharing online. Doctors have multiple roles including as medical experts, communicators, collaborators, managers, health advocates, scholars, and professionals providing high-quality care. New curriculum models focus on communication skills, preparation for practice, teamwork, and evidence-based practice. Health planning is crucial given concerns over efficient resource use and involves situational analysis, priority setting, option appraisal, programming and budgeting, implementation and monitoring, and evaluation. Primary health care and its essential components are also outlined.