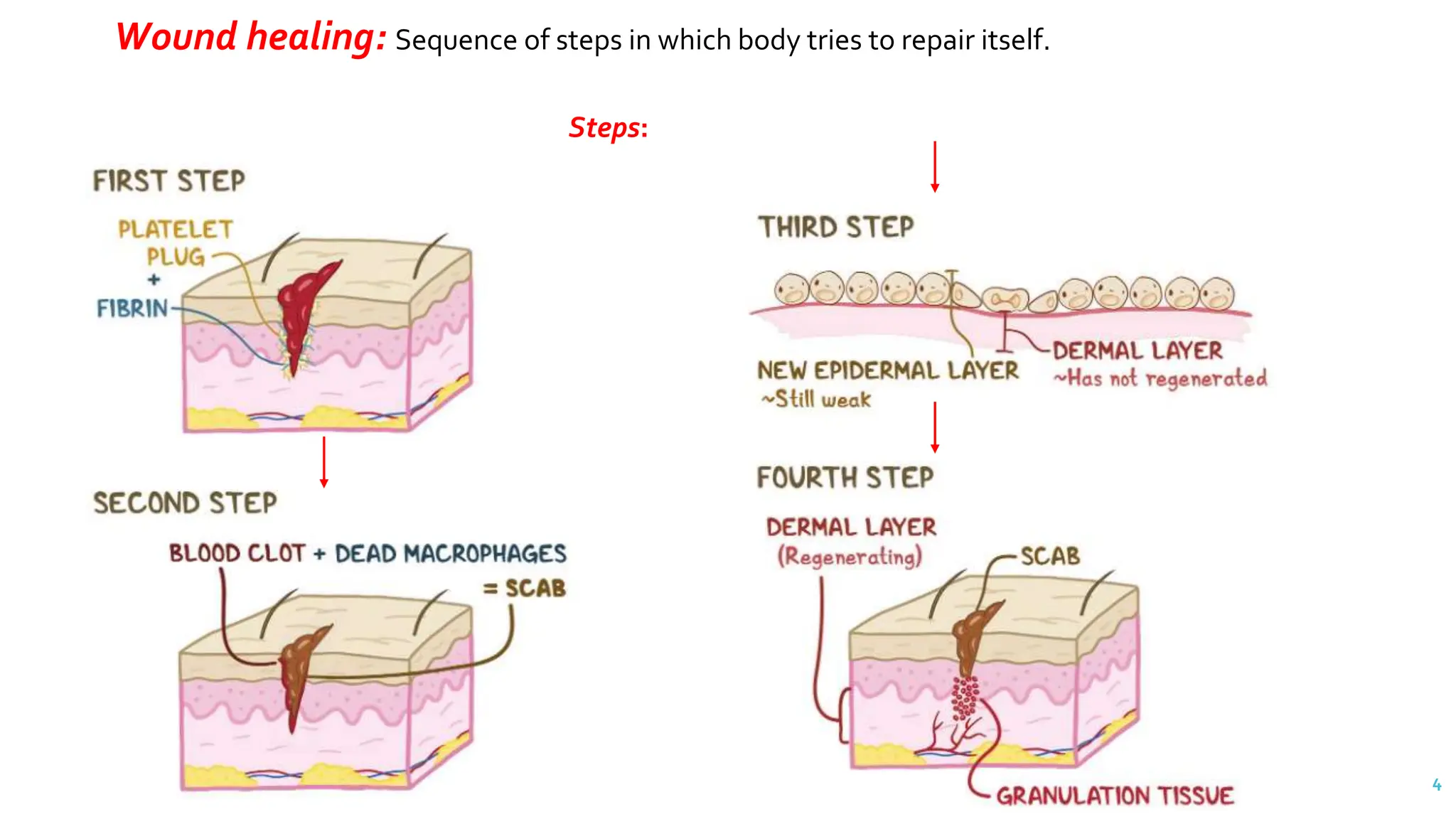
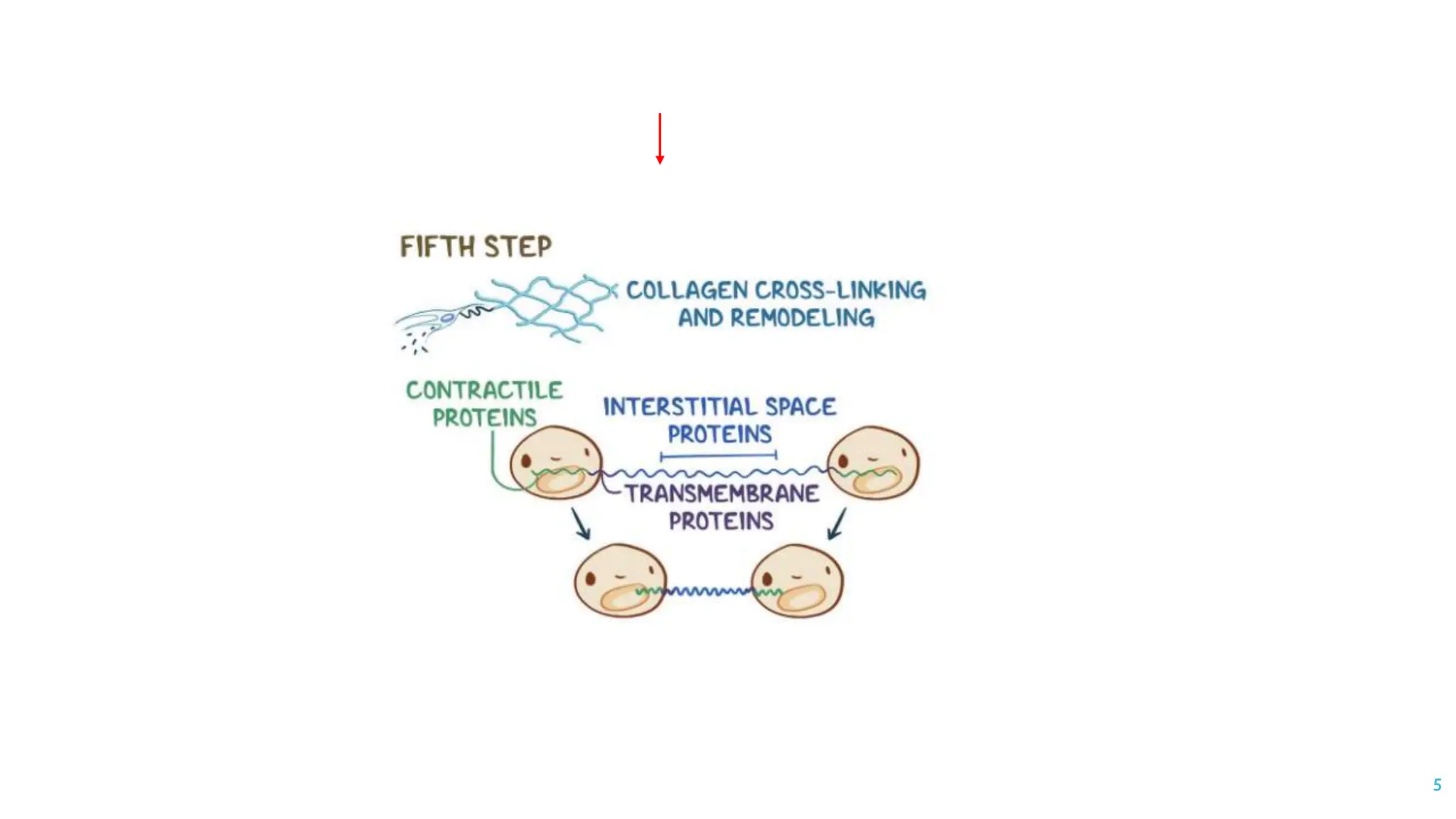
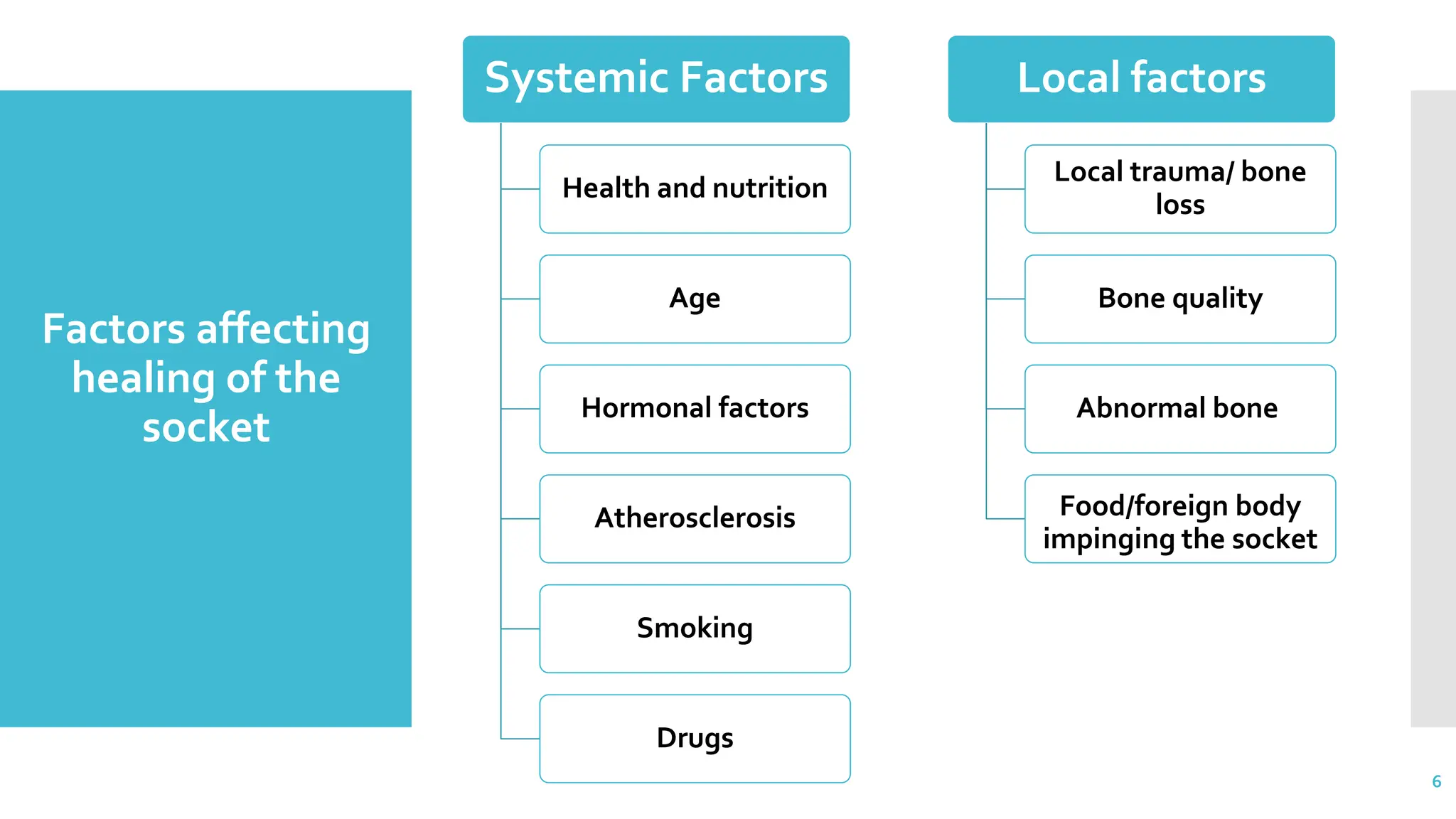
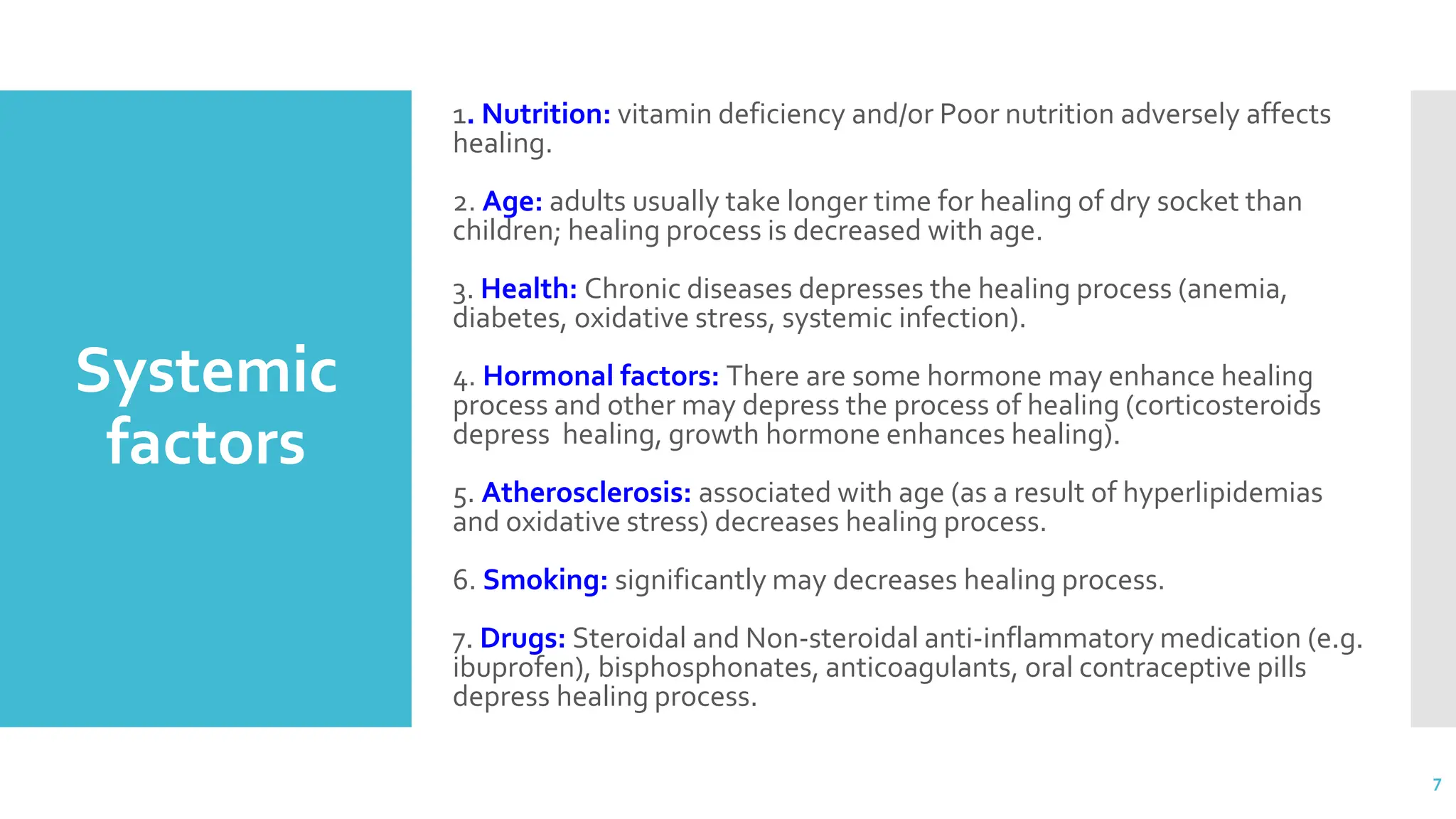
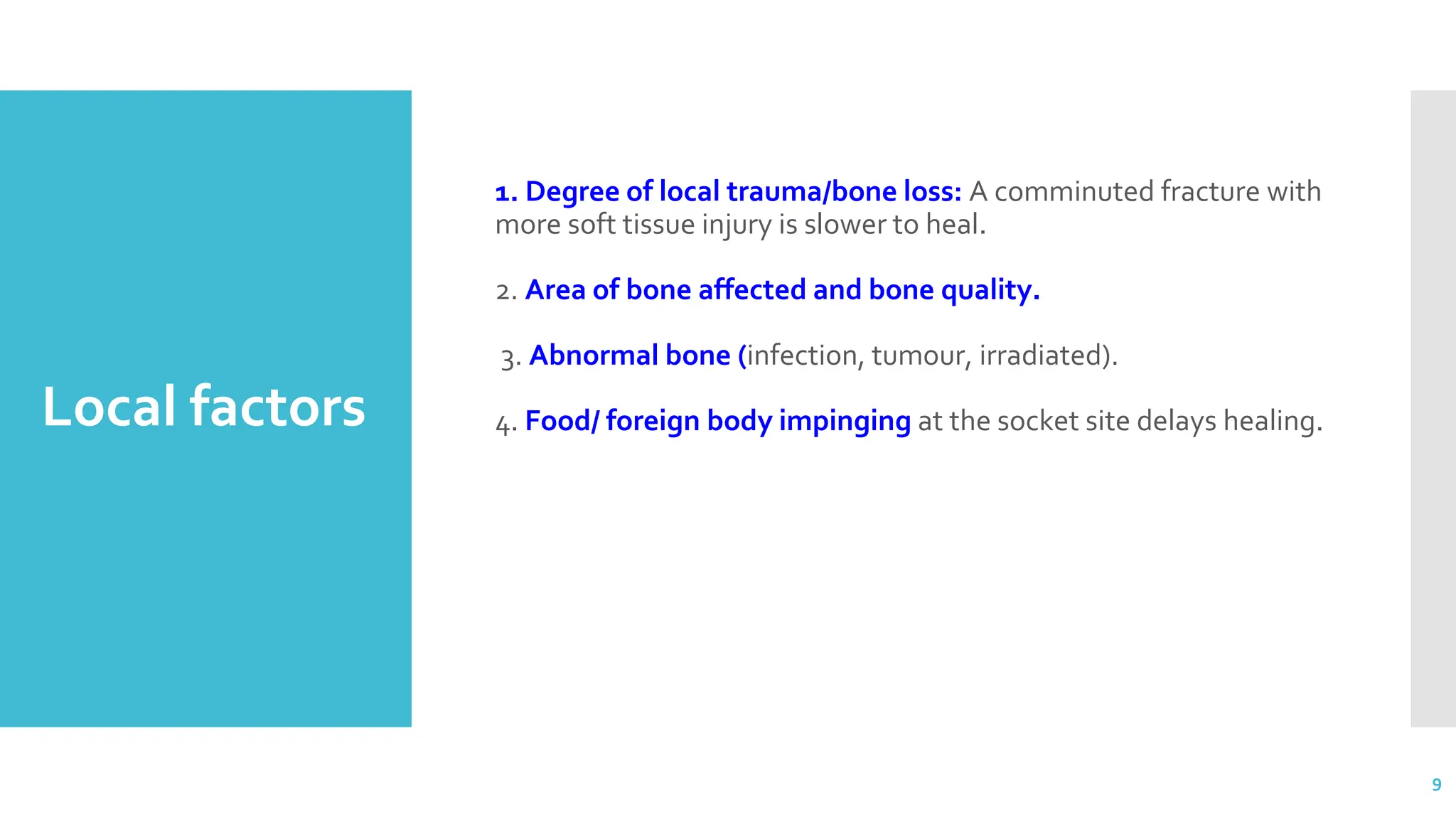
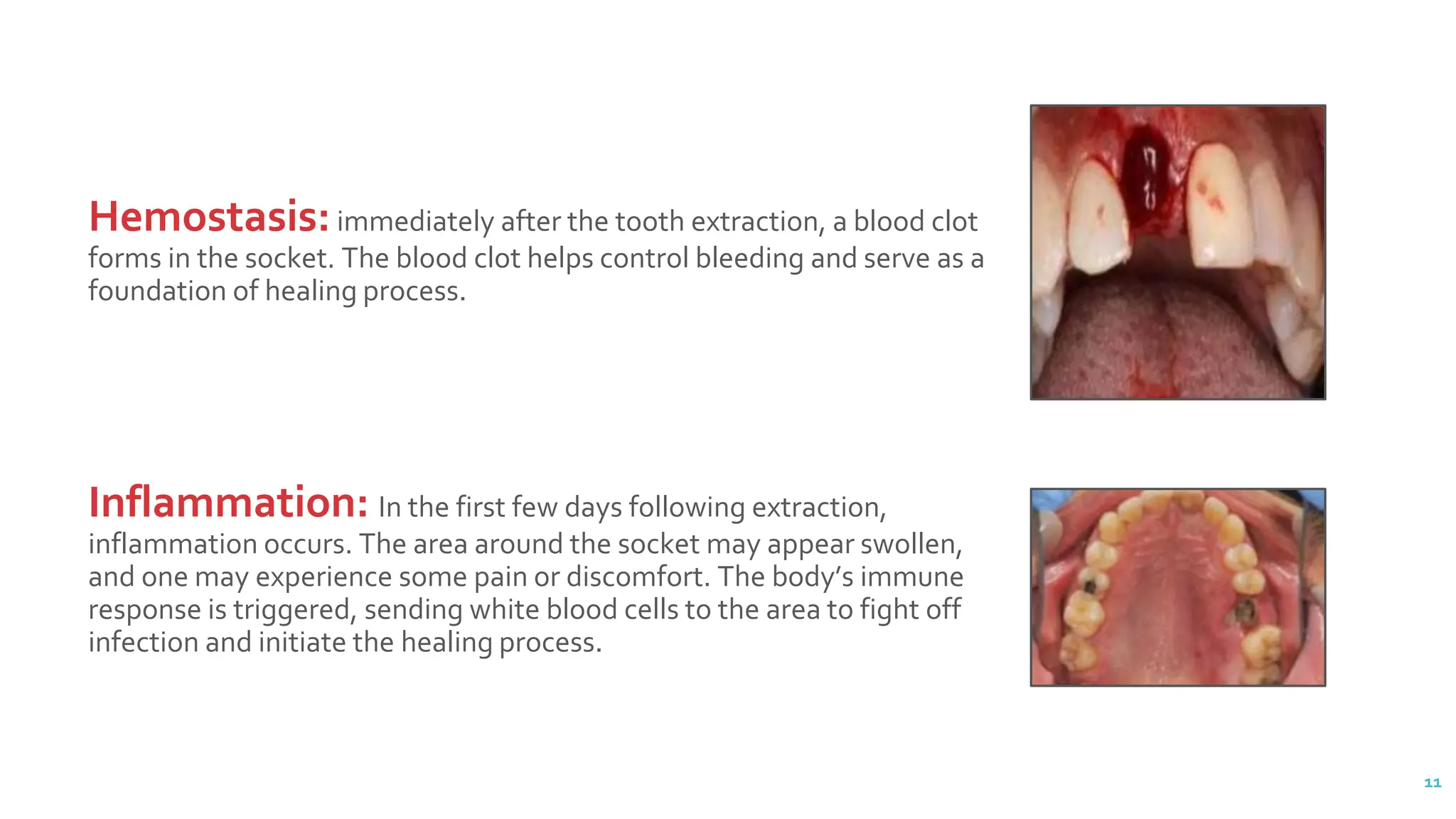
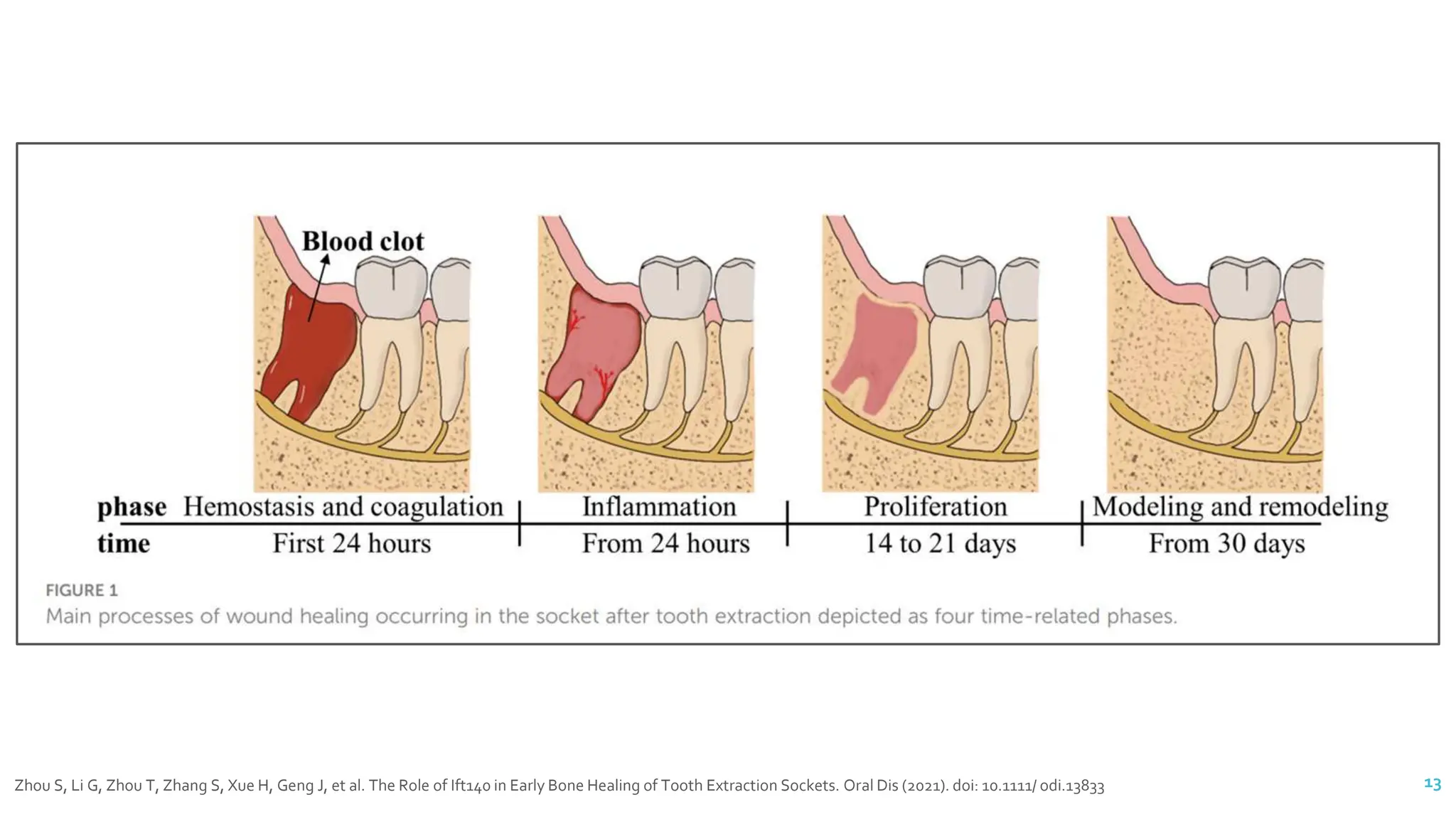
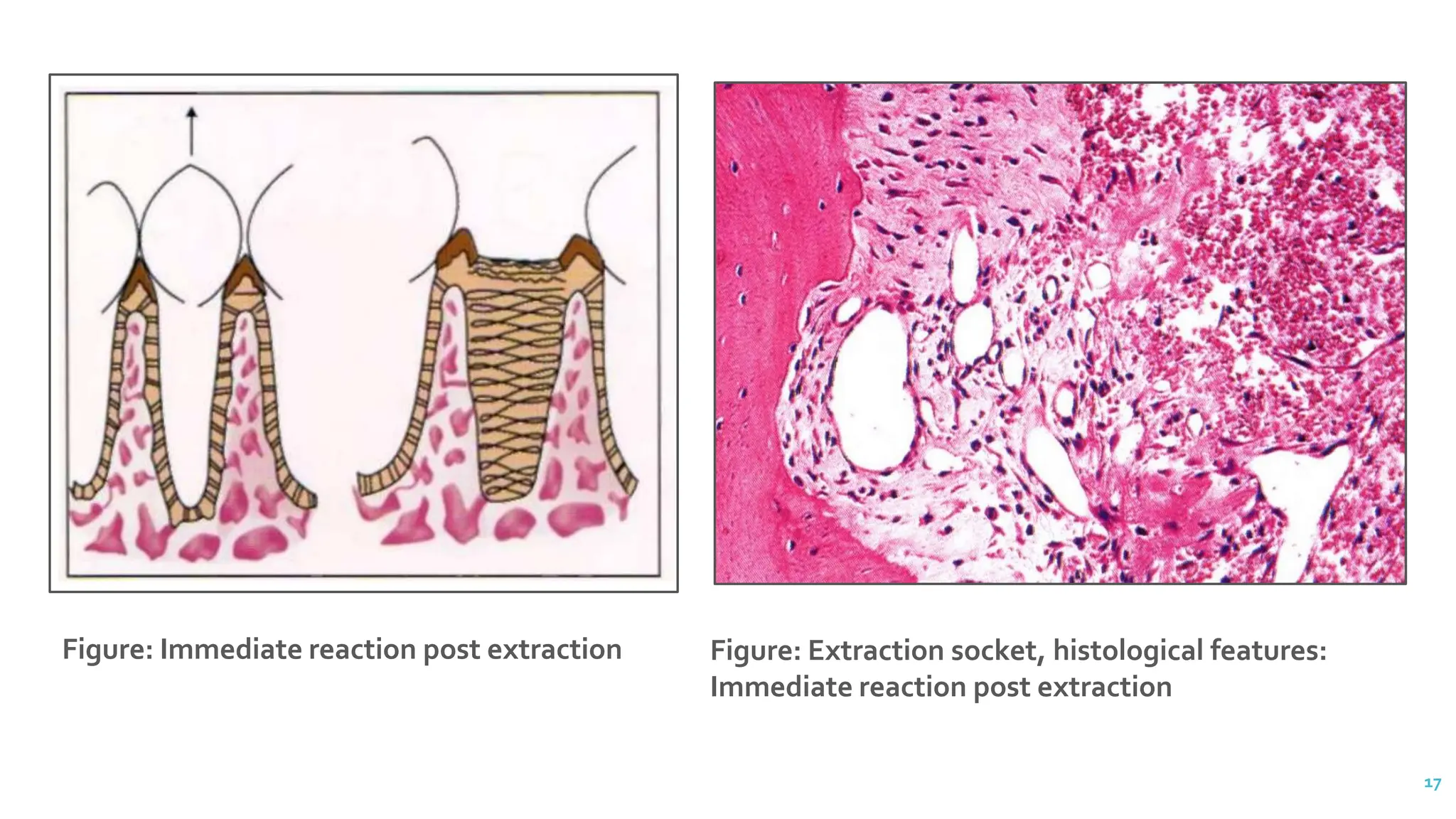
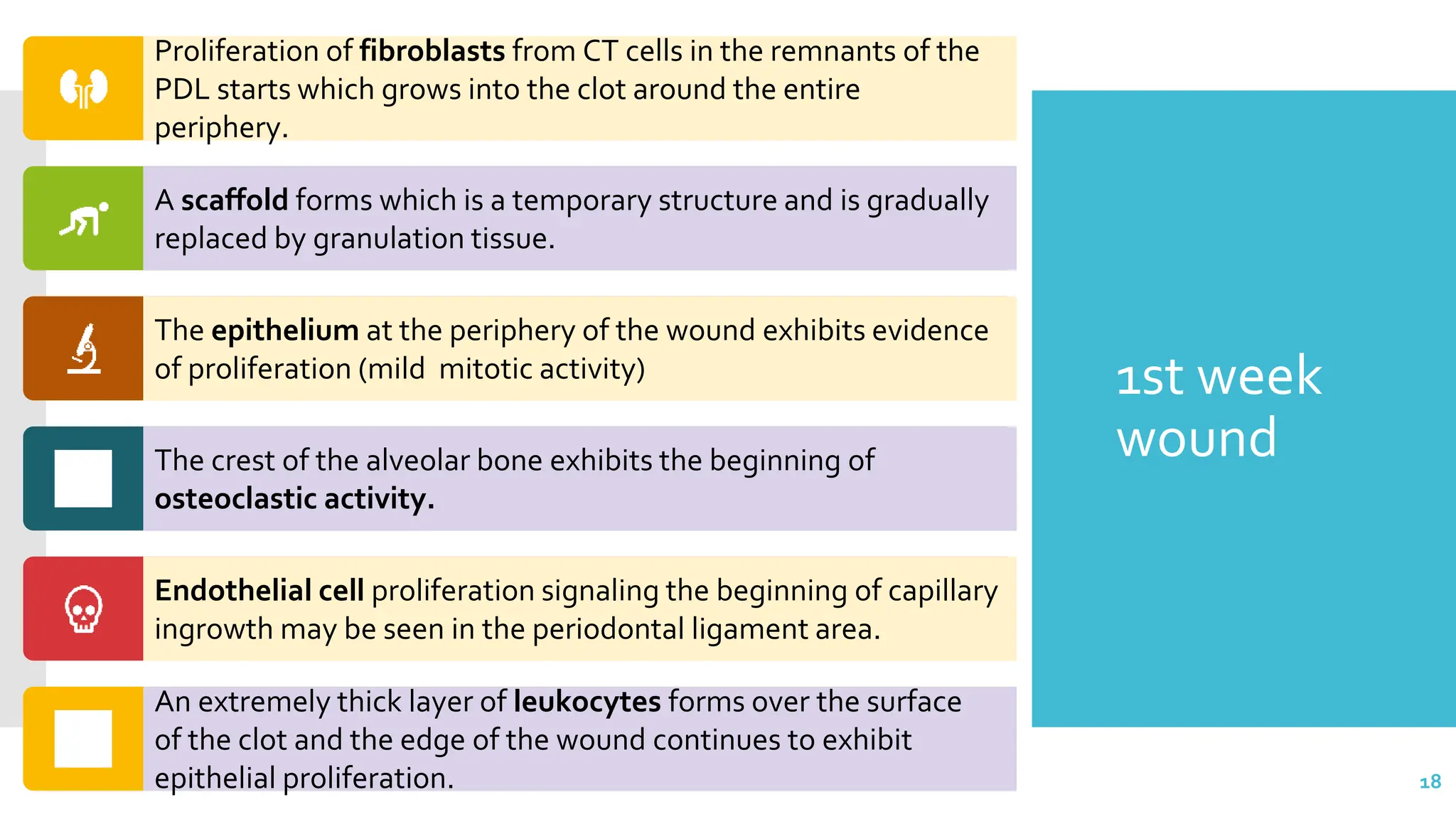
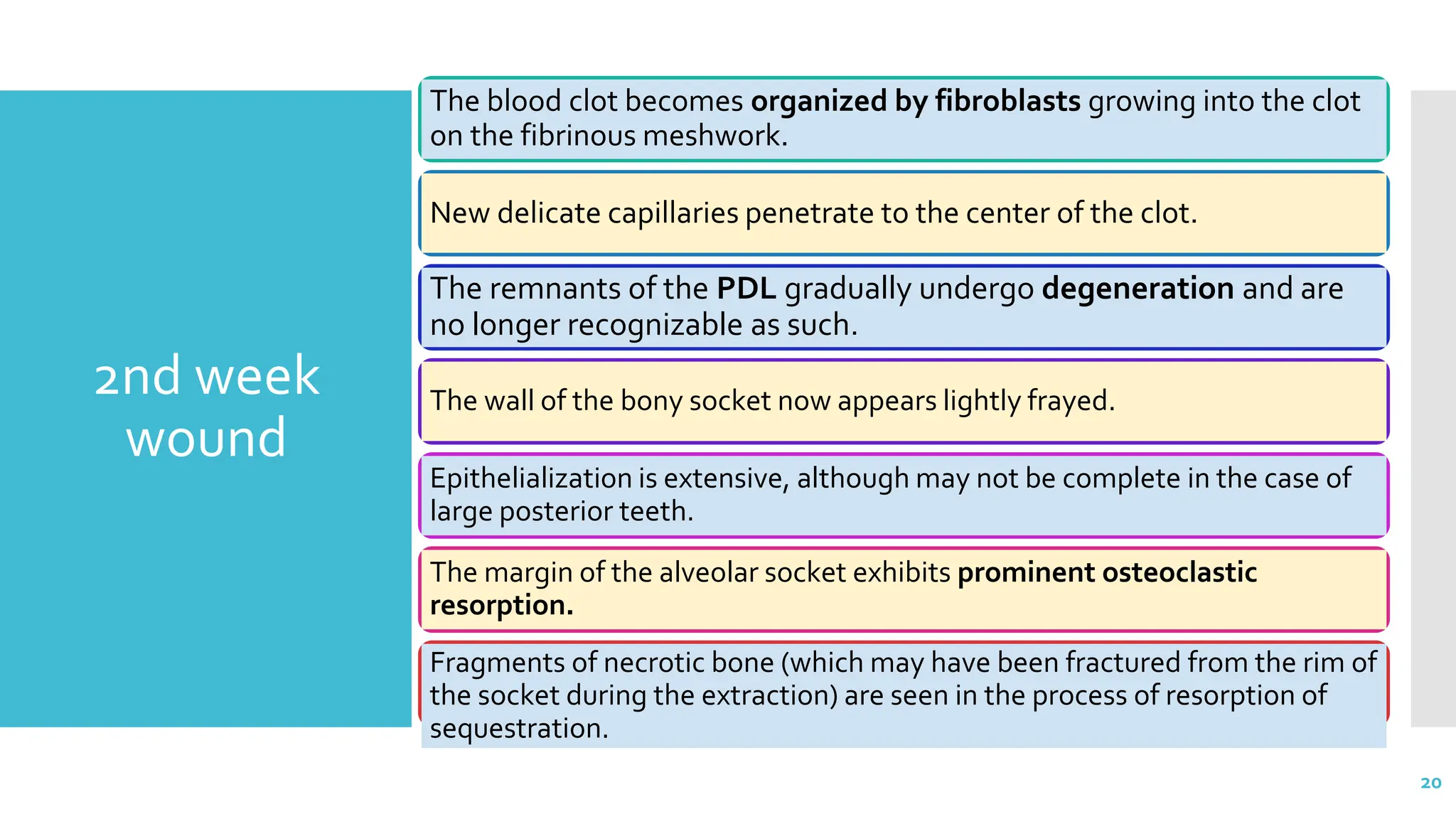
1) The document discusses the healing process of extraction sockets, including the typical stages (hemostasis, inflammation, granulation tissue formation, epithelialization), factors that can affect healing, and potential complications.
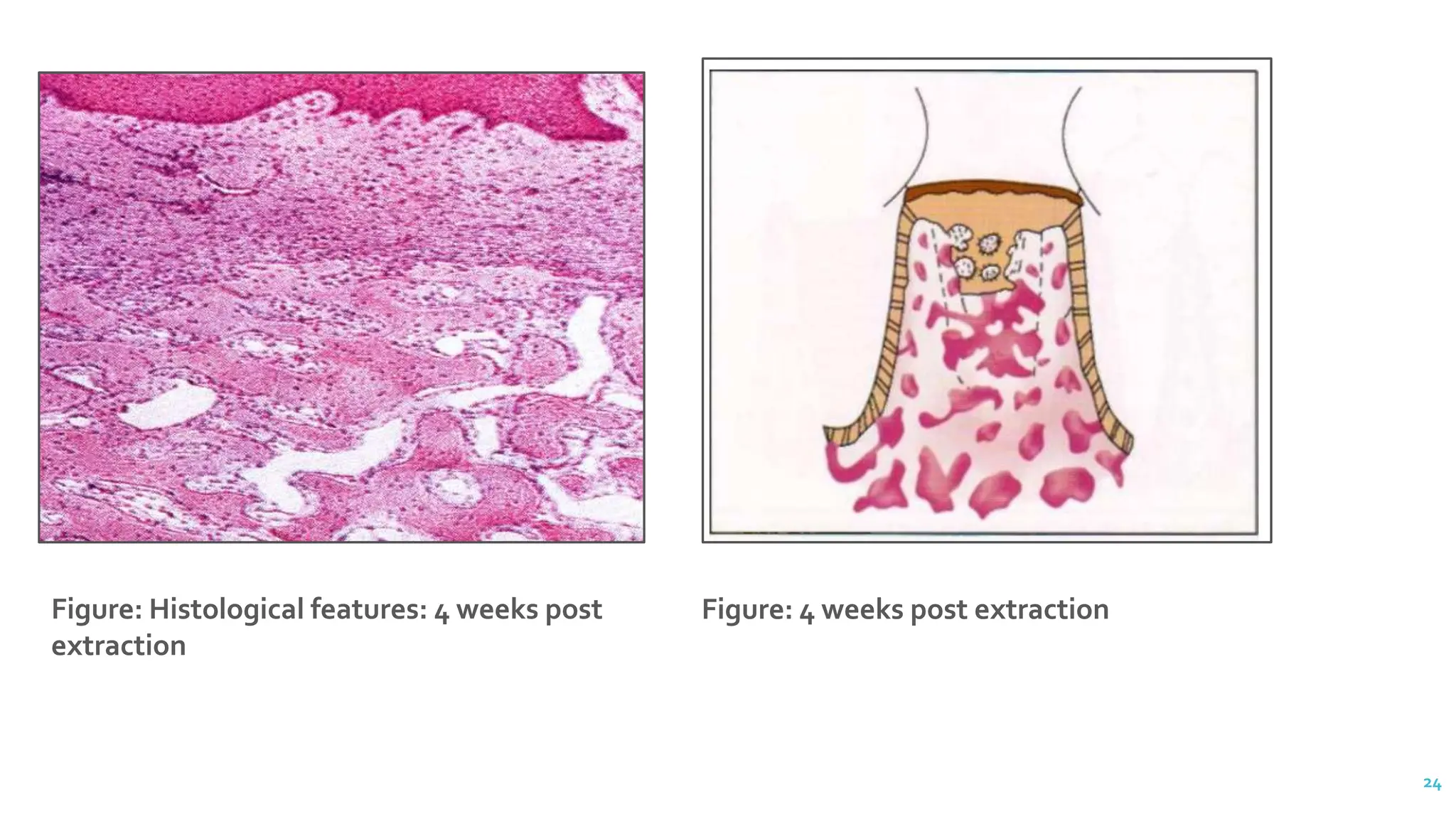
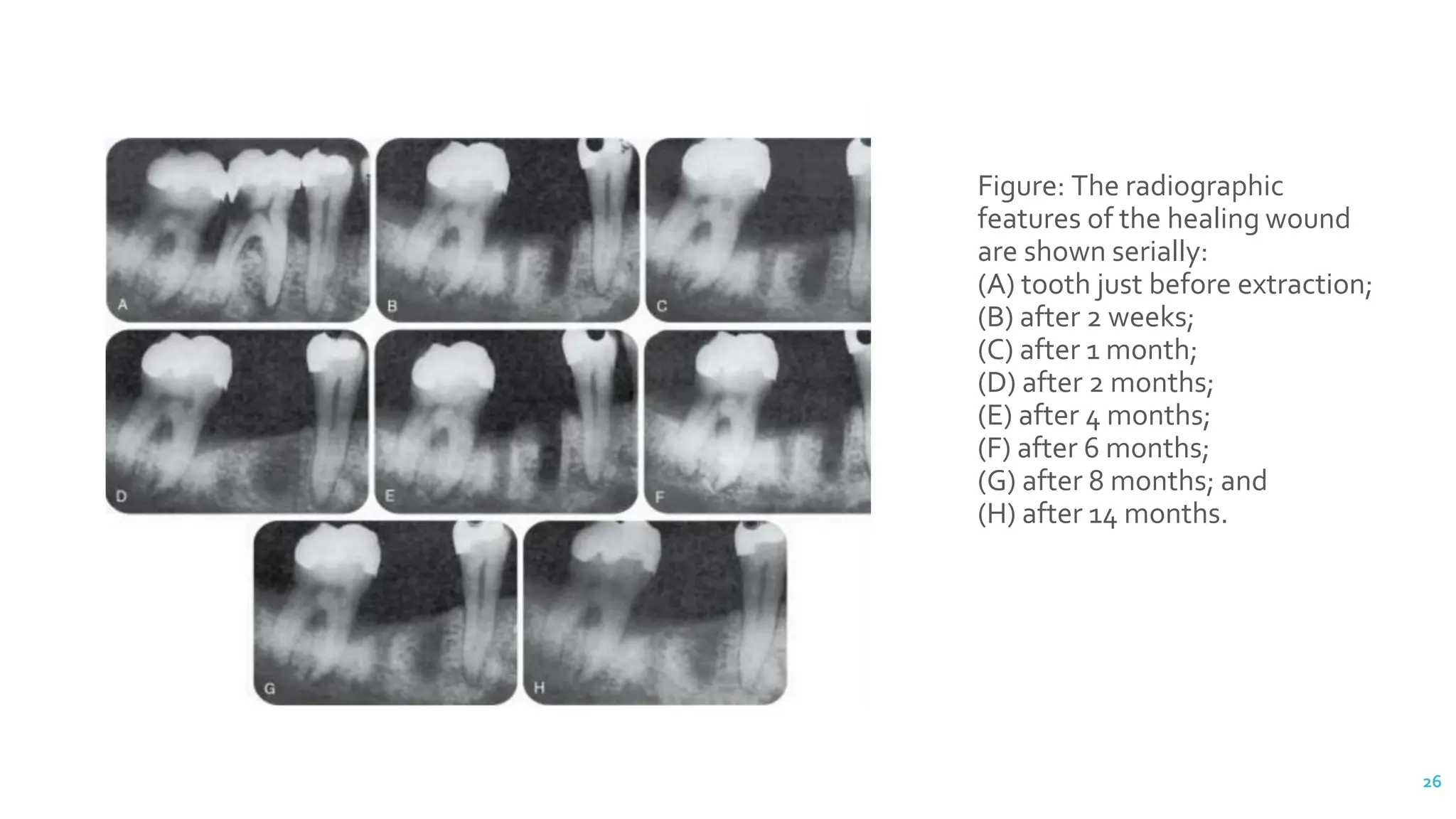
2) It describes the normal sequence of healing over 4 weeks, including clot organization, new bone formation, and bone remodeling.
3) The most common complication is dry socket, which results from disintegration of the blood clot exposing raw bone and causes severe pain for 7-10 days.