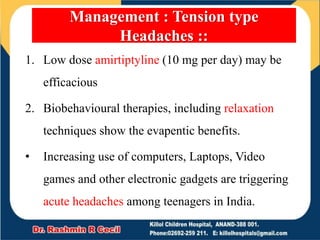
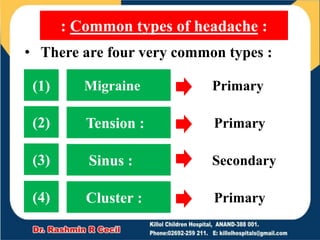
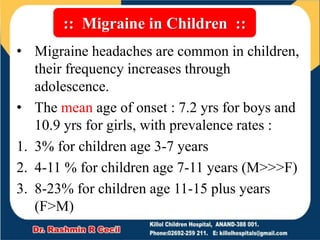
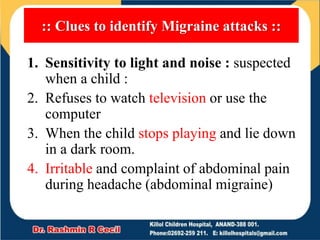
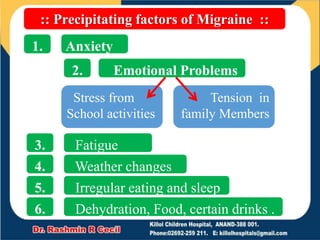
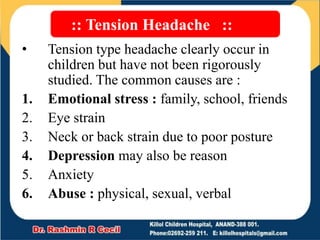
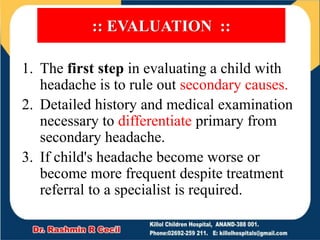
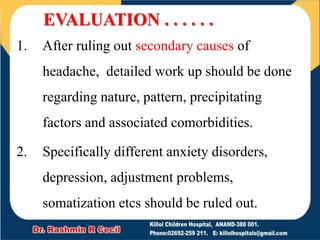
This document discusses headaches in children. It classifies headaches as either primary or secondary. The most common primary headaches in children are migraine, tension headache, and cluster headache. Migraines affect 3-23% of children and symptoms include throbbing pain, sensitivity to light/sound, and nausea. Tension headaches are caused by emotional or physical stress and eye strain. The document provides guidelines for evaluating and managing common childhood headaches.
![• [1] Primary headache :
• Headache is considered primary when a
disease or other medical condition does
not cause the headache.
• Primary headaches are benign, chronic
and not life threatening.
• Primary headaches fall into three main
types:
1. Migraine (16%)
2. Tension headache (69%)
3. Cluster headache](https://image.slidesharecdn.com/headacheinchildren23-210726063233/85/Headache-in-children-4-320.jpg)
![• [2] Secondary headache :
• Secondary headaches are due to
underlying medical conditions.
• It may be resulting from life threatening
diseases, early diagnosis is essential
• Most common causes are :
1. Infectious (63%) Sinusitis, Pharyngitis,
ear infections
2. Vascular
3. Traumatic (49%)
4. Mass lession](https://image.slidesharecdn.com/headacheinchildren23-210726063233/85/Headache-in-children-5-320.jpg)
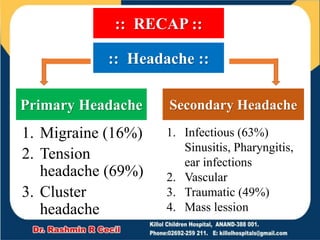
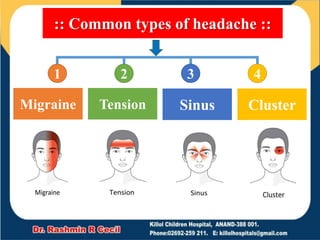
![• [1] Migraine :
• Symptoms:
1. Pain in the face or neck,
2. Throbbing in one area,
3. Sensitivity to light and sound,
4. Nausea, distorted vision
• Duration: 4 to 72 hours](https://image.slidesharecdn.com/headacheinchildren23-210726063233/85/Headache-in-children-10-320.jpg)
![• [2] Tension :
• Symptoms :
• Dull pain on either side of the head,
and pressure across the forehead
• Duration: 30 minutes to several hours
• [3] Sinus :
• Symptoms :
• Pain in the face, sinuses, eyes, ears or
forehead. Congestion, itching, runny nose,
fever, swelling in the face.
• Duration : several days to weeks (if treated)](https://image.slidesharecdn.com/headacheinchildren23-210726063233/85/Headache-in-children-11-320.jpg)
![• [4] Cluster :
• Symptoms :
1. severe pain on one side of the head,
2. usually around the eye,
3. accompanied with a drooping eyelid,
4. small pupil, tearing, runny nose or
redness on the same side of the head
• Duration :
• Can last for weeks or several months,
usually followed by a period of
remission that can last for several
months or several years.](https://image.slidesharecdn.com/headacheinchildren23-210726063233/85/Headache-in-children-12-320.jpg)
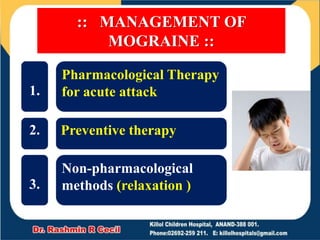
![1. Intermittent use of oral analgesic is the
mainstay of treatment; Both Ibuprofen and
acetaminophen have been shown to be safe and
effective
2. Sumatriptan is the only 5HT1 agonist that has
proven effective for the treatment of children
and with migraine with the nasal spray having
the most favorable profile
3. Narcotics should be avoided
4. Nausea and vomiting can be relieved by
antiemetic agents
[1] Pharmacological therapy for accute
attack ::](https://image.slidesharecdn.com/headacheinchildren23-210726063233/85/Headache-in-children-25-320.jpg)
![1. Use of prophylactic agents Propranolol
and Flunazine should be reserved for
children with frequent or disabling
migraine headaches.
2. The Optium duration of prophylactic
therapy is uncertain.
3. Data are limited on the effectiveness of
preventive agents in children
[2] Preventive therapy ::](https://image.slidesharecdn.com/headacheinchildren23-210726063233/85/Headache-in-children-26-320.jpg)
![1. Education
2. Relaxation therapy
3. Stress management
4. Sleep Hygiene
5. Eliminate triggers
6. Regular Exercise
[3] Non-Pharmacological methods :](https://image.slidesharecdn.com/headacheinchildren23-210726063233/85/Headache-in-children-27-320.jpg)