This document summarizes a presentation on pediatric headache and migraine management in the emergency department. It discusses:
1) Common differential diagnoses for pediatric headache in the ED including primary headaches like migraine and secondary headaches.
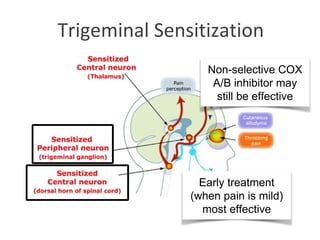
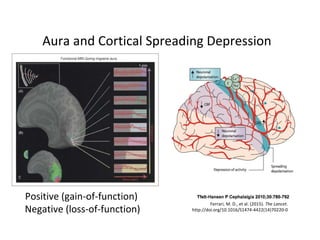
2) An overview of migraine physiology and the trigeminovascular system. Cortical spreading depression may trigger migraines by activating the trigeminovascular system.
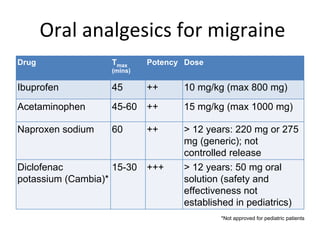
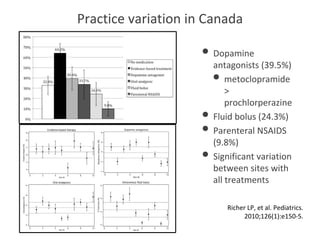
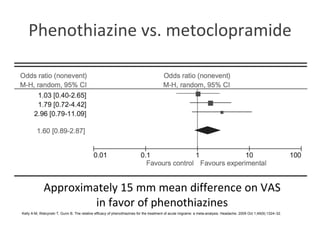
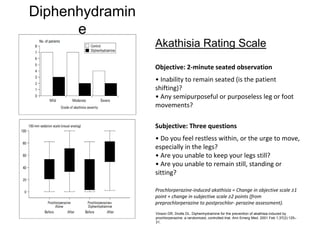
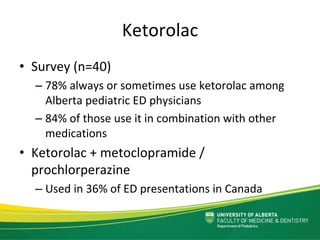
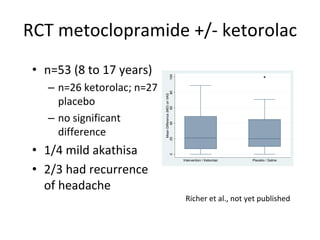
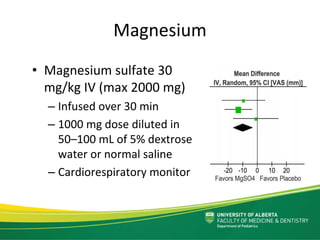
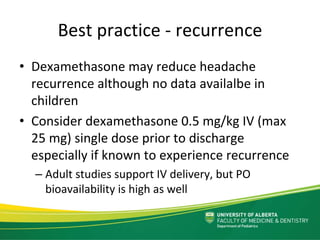
3) Current evidence and controversies around migraine treatment in the ED, including oral, nasal, and subcutaneous triptan therapies as well as novel drug targets in development. Fluid bolus therapy and dopamine antagonists are commonly used but practice varies significantly between sites.












![ACR Appropriateness Criteria for Child
with Headache
Primary Headache
• No imaging is indicated for typical
migraine.
• In ophthalmologic migraine with focal
neurologic symptoms of unilateral
ptosis or complete third‐nerve palsy,
MRI is recommended.
• MRI is also recommended for patients
with miscellaneous findings such as
vertigo, basilar artery migraine
syndrome, persistent confusion
migraine syndrome, progressive chronic
headache, or hemiplegic migraine.
• MRI should be performed for patients
with seizures and postictal headaches.
Secondary Headache
• If neurologic signs or symptoms of increased
intracranial pressure are present, MRI is
recommended. If MRI is not available or
there are problems with sedation, CT should
be performed.
• CT of the head without intravenous contrast
is recommended for sudden severe
headaches (thunderclap headaches).
• If subarachnoid hemorrhage is detected, CT
or conventional angiography should be
performed. MRA is also appropriate but is
generally considered less sensitive in
detecting small aneurysms.
• If intracranial hemorrhage is present, MRI of
the brain should be performed if possible.
Obtaining a concomitant MRA is
recommended.
Hayes LL, Coley BD, Karmazyn B et al. American College of Radiology. ACR Appropriateness Criteria. Headache—child.
Reston (VA): ACR [Internet]. 2012[cited 2015 Jun 25]; 8. Available from: https://acsearch.acr.org/docs/69439/Narrative/](https://image.slidesharecdn.com/dr-151109134702-lva1-app6891/85/La-migraine-16-320.jpg)
![Appropriateness Rating
Category
N Imaged % Important
Abnormalities
Incidental
Abnormalities
Usually not appropriate 72 4 6% 0 1
May be appropriate 13 8 61% 1 1
Usually appropriate 10 8 80% 1 3
Imaging Audit
- 95 patient visits sampled
- Diagnosis: headache in 35, migraine in 53, meningeal infection
in 1, neoplasm with hydrocephalus in 1, metabolic disease in 1
and other non-relevant conditions in 4
- 4 patients imaged did not meet any appropriateness criteria,
but each had prior neurosurgery
Hayes LL, Coley BD, Karmazyn B et al. American College of Radiology. ACR Appropriateness Criteria. Headache—child.
Reston (VA): ACR [Internet]. 2012[cited 2015 Jun 25]; 8. Available from: https://acsearch.acr.org/docs/69439/Narrative/](https://image.slidesharecdn.com/dr-151109134702-lva1-app6891/85/La-migraine-18-320.jpg)