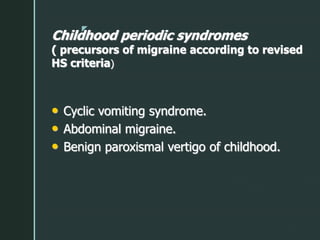
1. Migraine is a common type of primary headache characterized by moderate to severe throbbing pain, nausea, photophobia, and phonophobia.
2. The classification and diagnostic criteria for migraine with and without aura according to the International Headache Society is described.
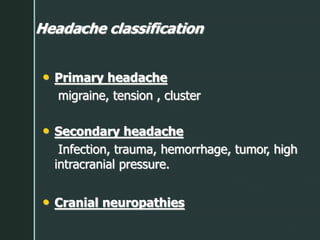
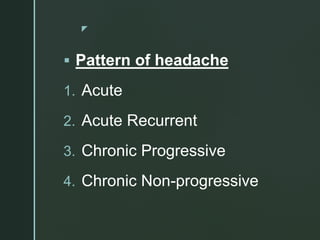
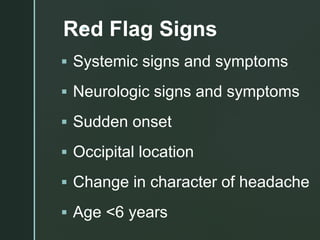
3. A thorough clinical evaluation including headache characteristics, triggers, family history, and examination for red flags is important to identify primary versus secondary headaches and guide further workup and treatment.