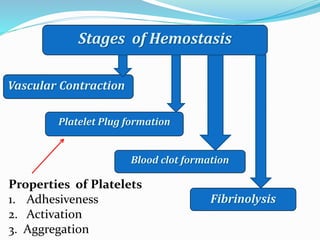
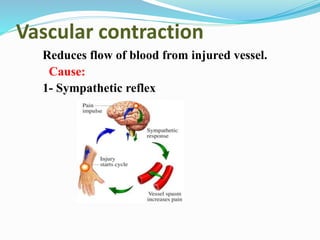
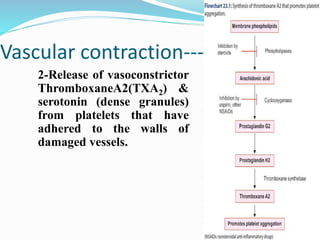
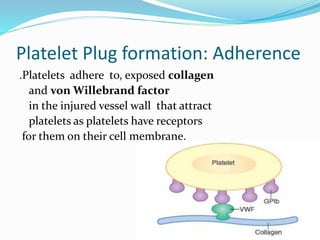
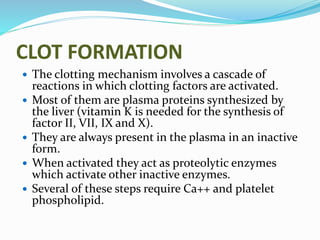
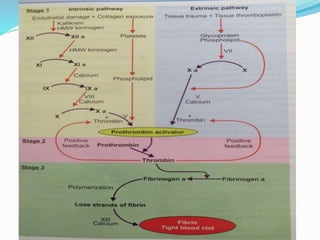
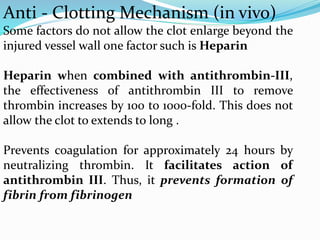
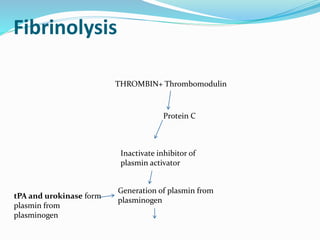
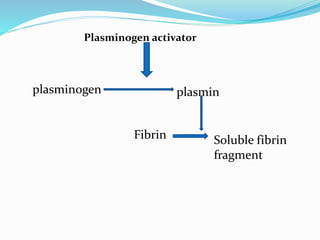
The document discusses hemostasis and bleeding disorders. It describes the three stages of hemostasis: vascular contraction, platelet plug formation, and blood clot formation. Thirteen coagulation factors involved in clot formation are also listed. Mechanisms of fibrinolysis, anti-clotting, and three main types of bleeding disorders - hemophilia, purpura, and von Willebrand disease - are summarized. Hemophilia is caused by a deficiency of coagulation factor VIII, IX or XI and results in prolonged clotting time. Purpura is characterized by prolonged bleeding time and purpuric spots due to ruptured capillaries. Von Willebrand disease is caused by a deficiency of the von