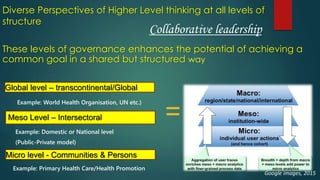
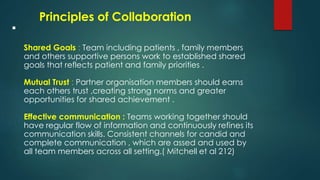
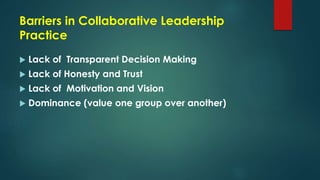
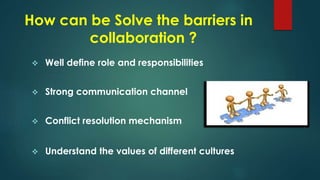
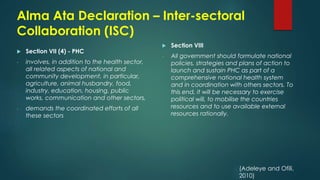
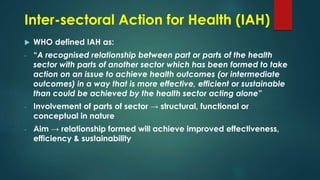
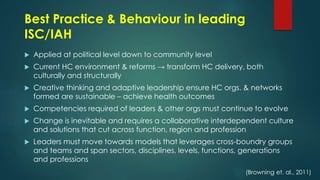
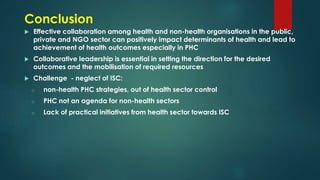
The document discusses collaboration between health and non-health organizations. It argues that collaborative leadership is important for achieving shared goals. Effective collaboration requires shared goals, mutual trust, and good communication. Barriers to collaboration include lack of transparency, trust and shared vision. Leaders can overcome barriers by employing participative leadership, transparent decision-making, and understanding different cultural perspectives. Examples of collaboration include school health programs and provision of basic infrastructure.