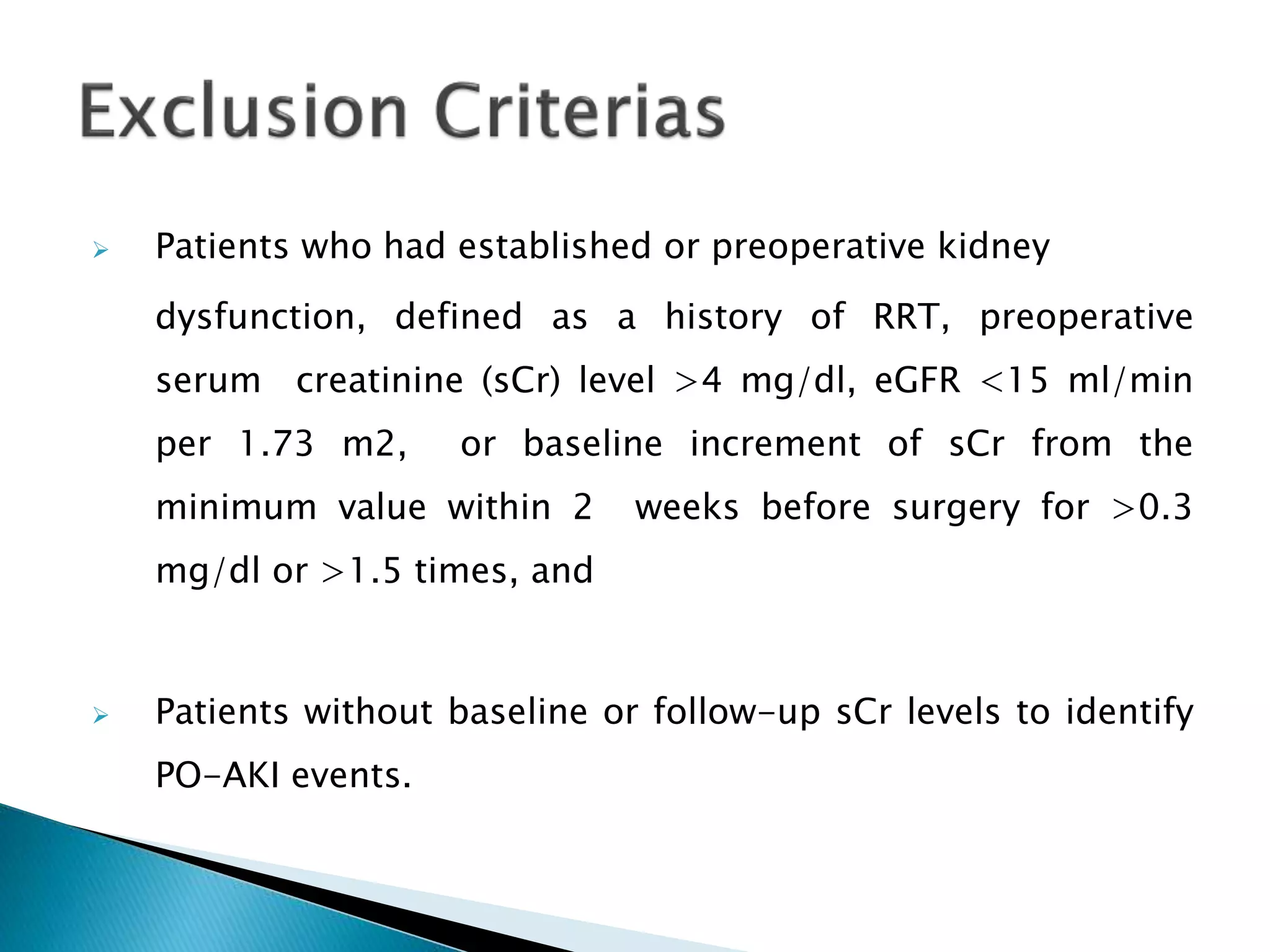
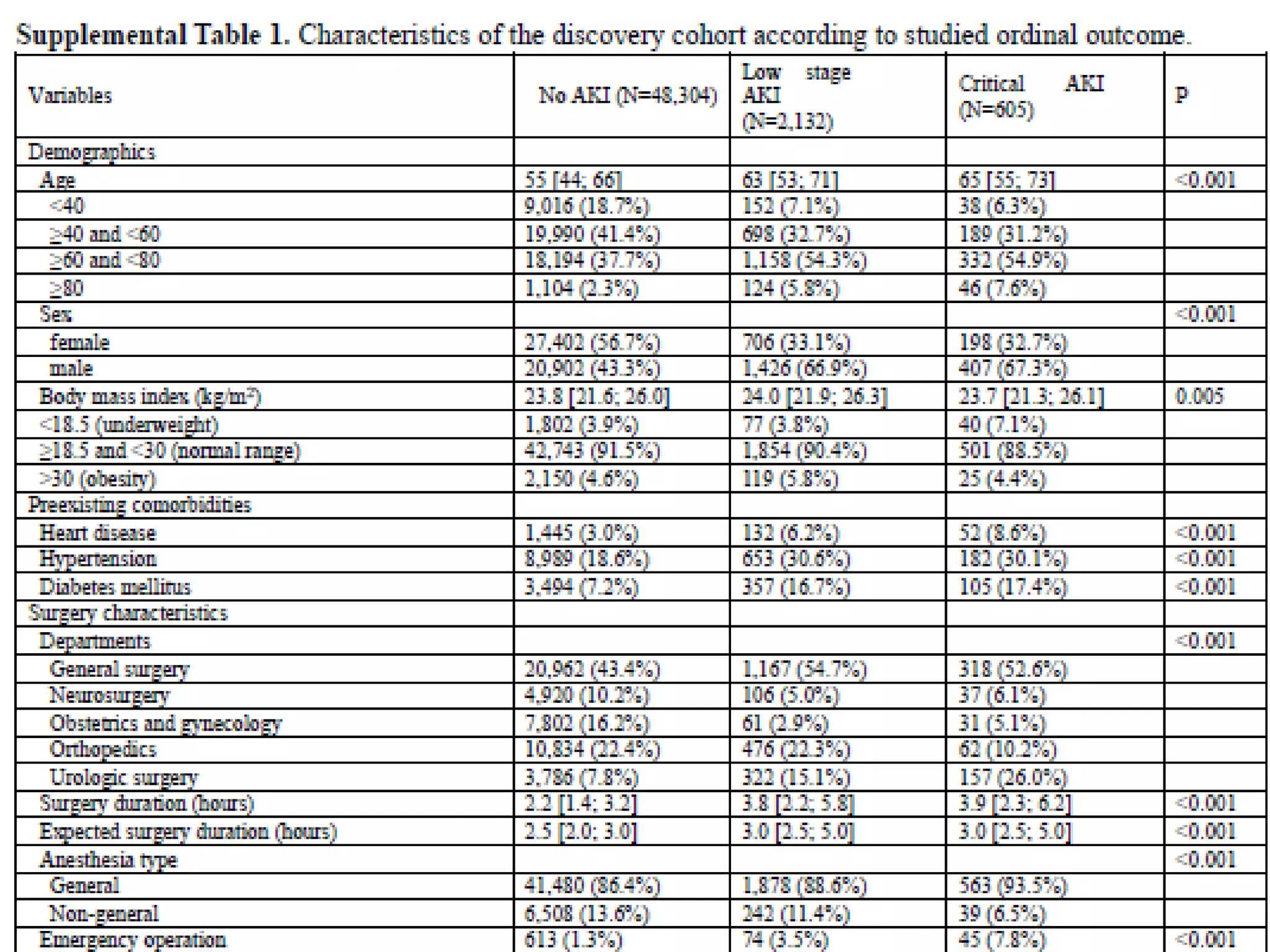
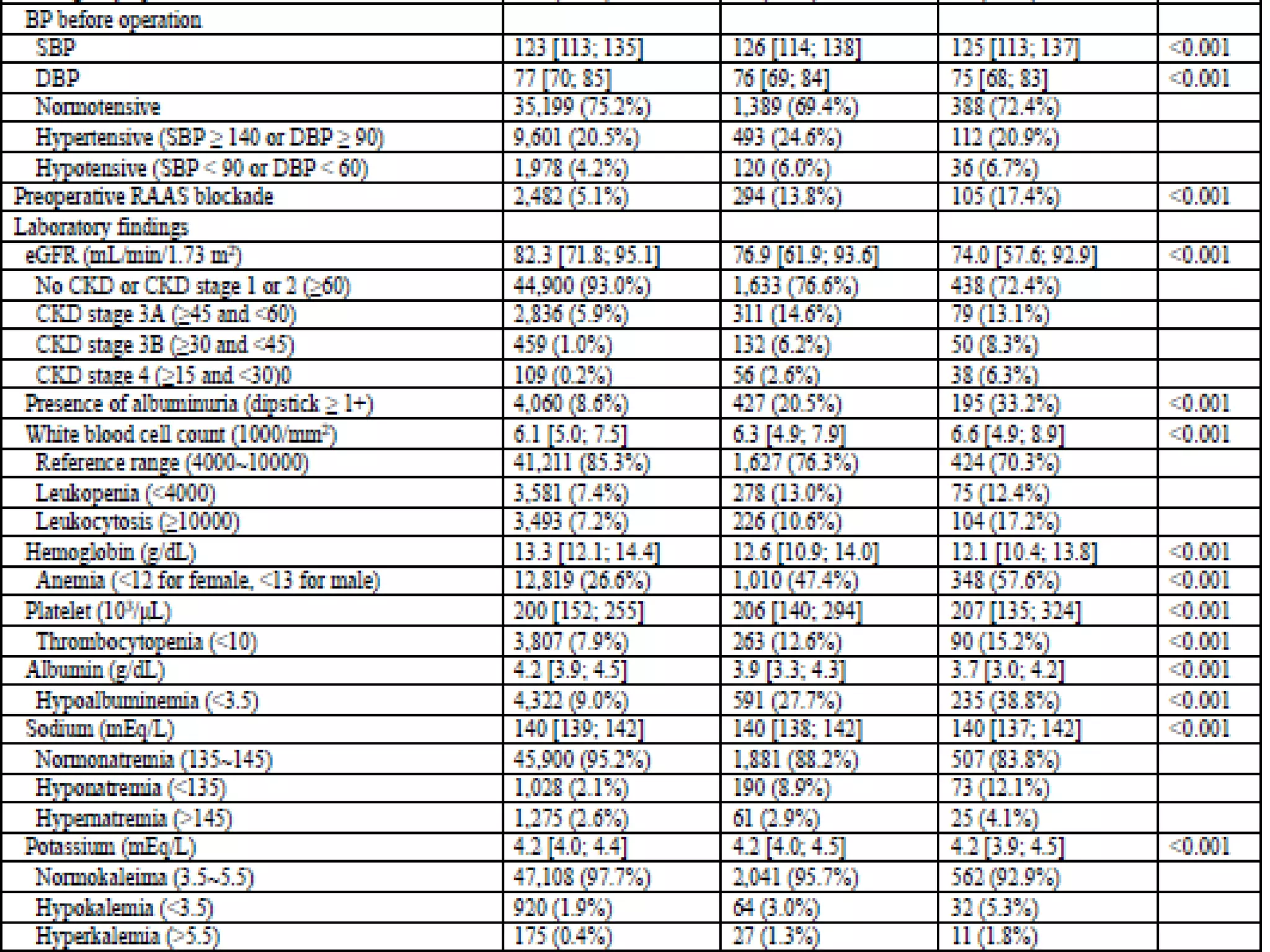
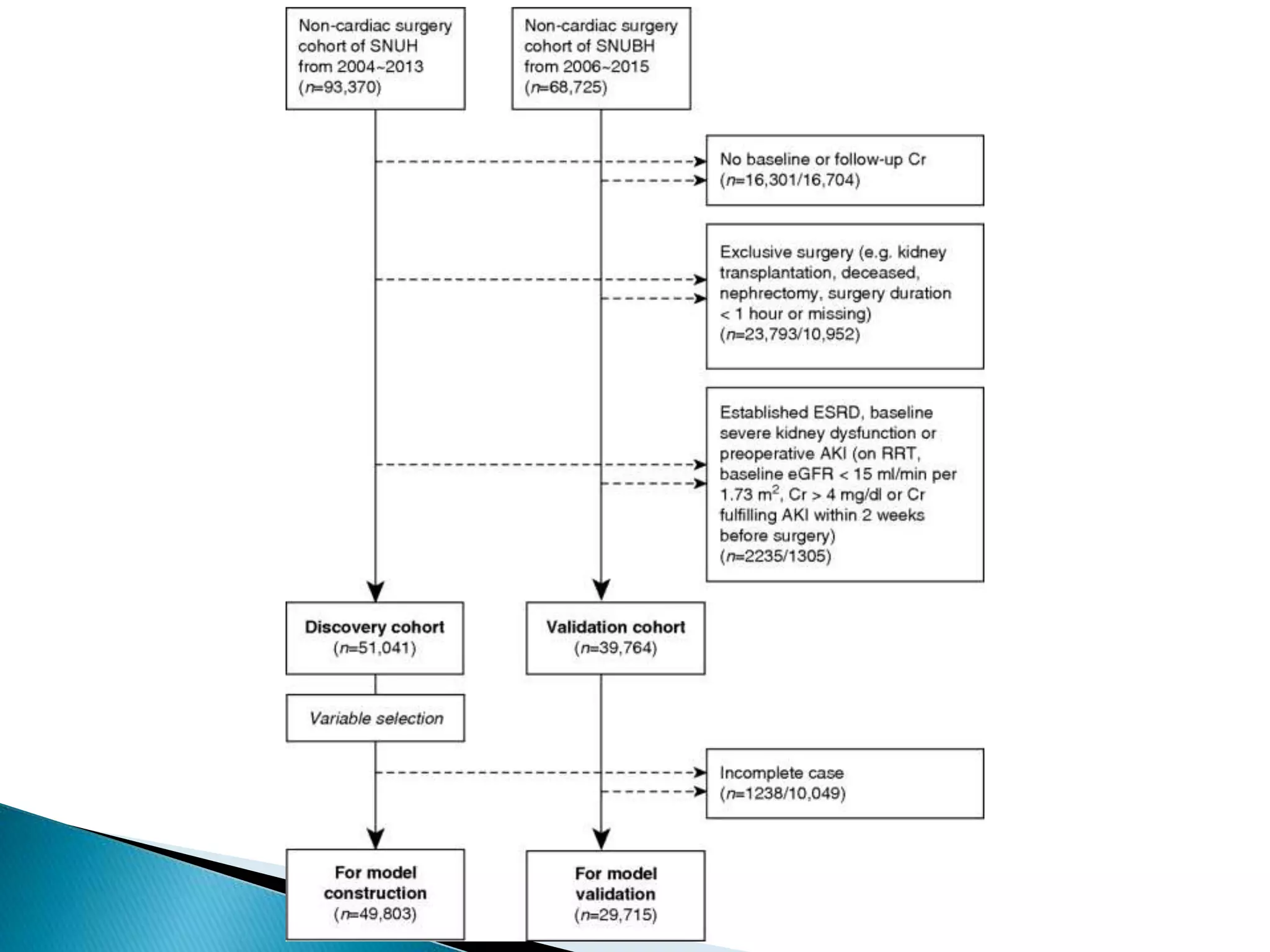
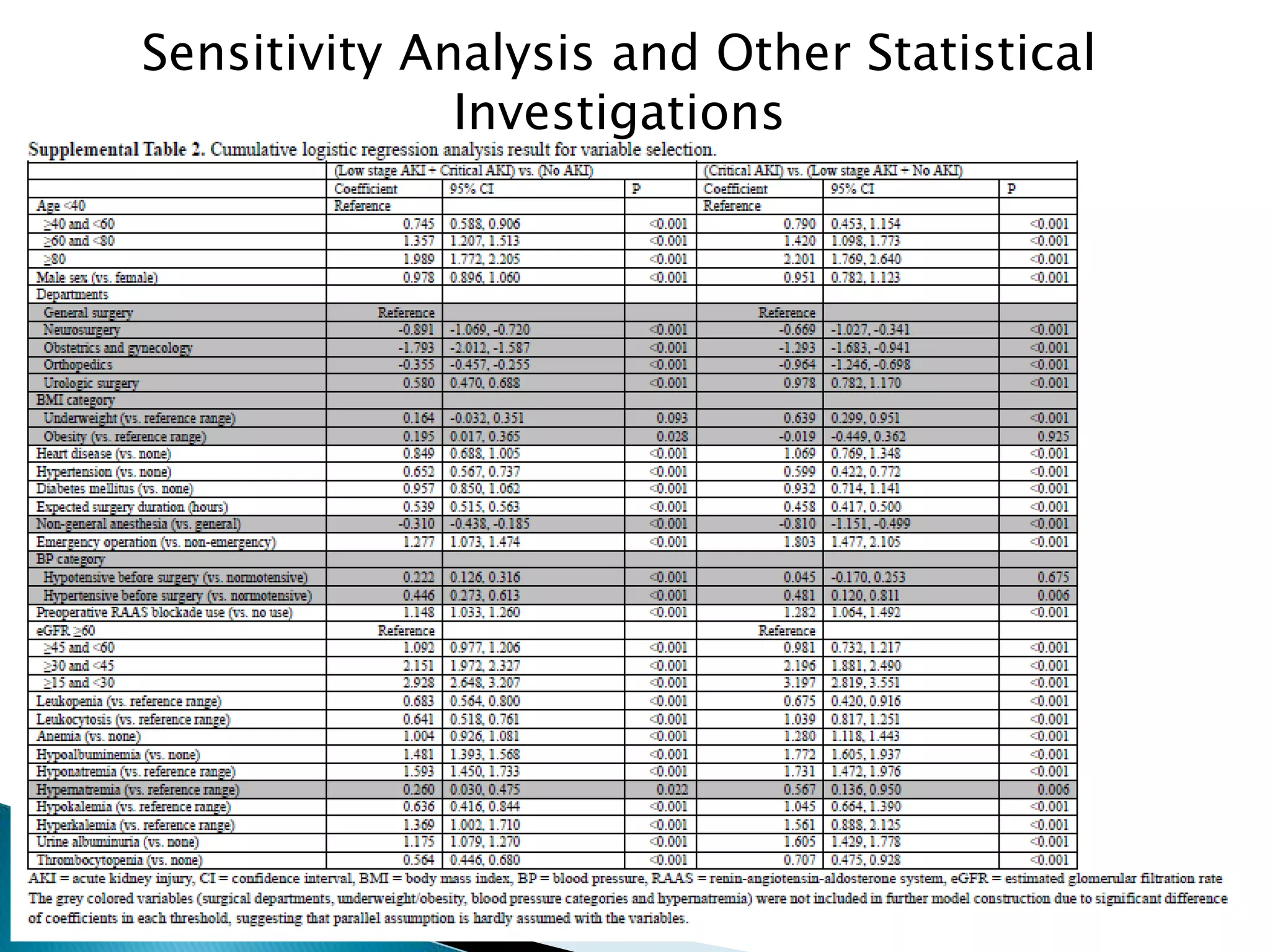
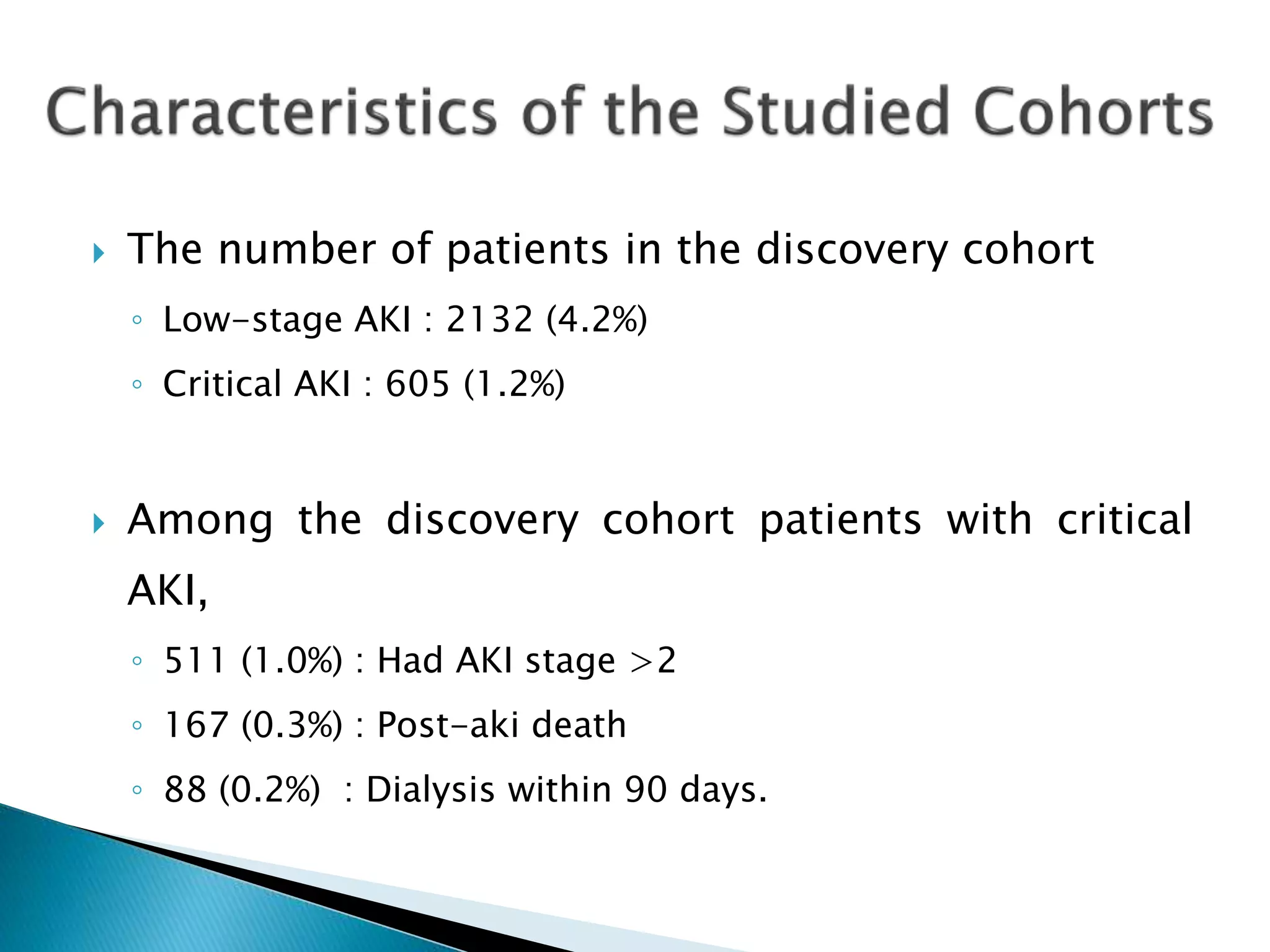
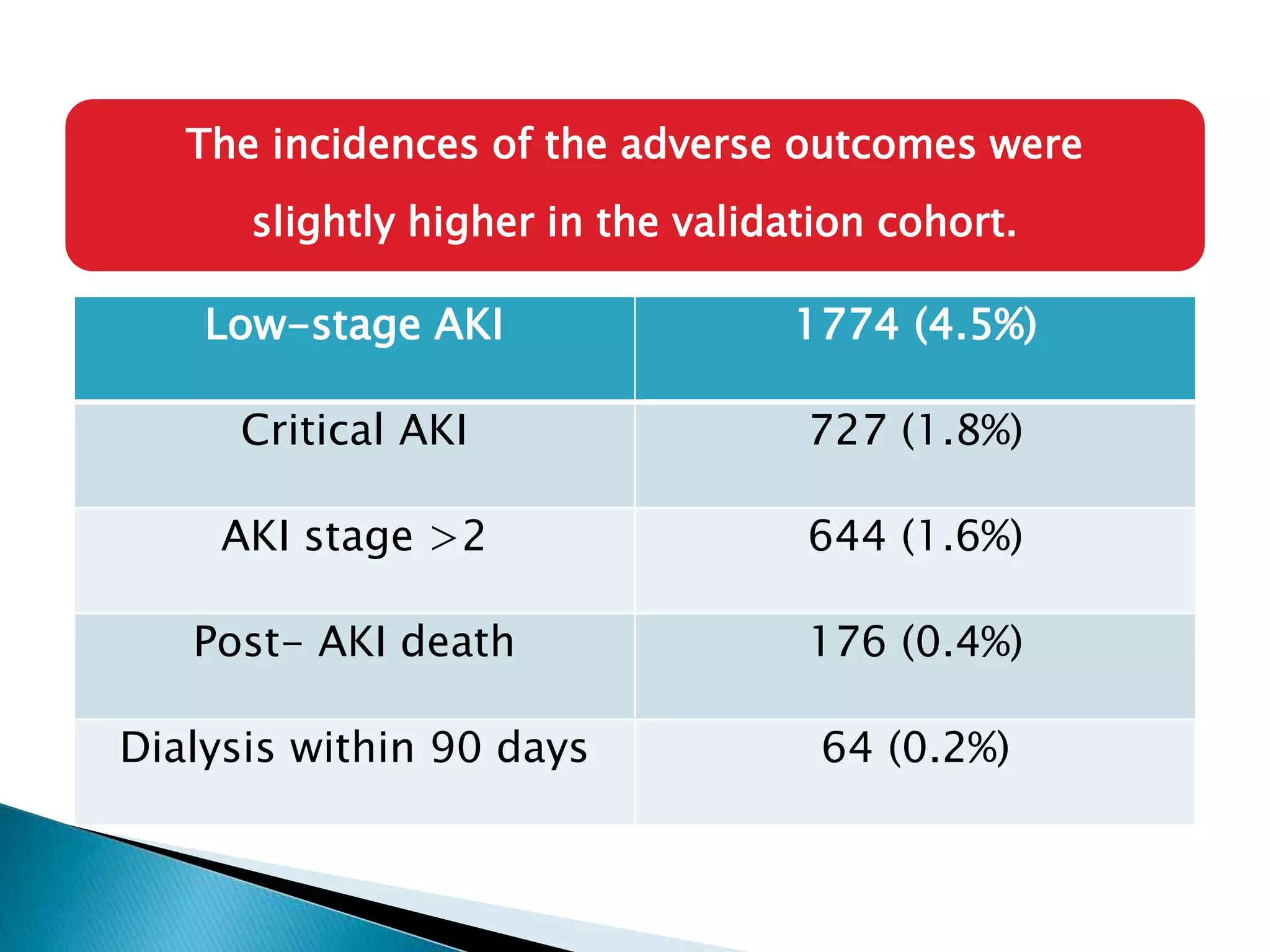
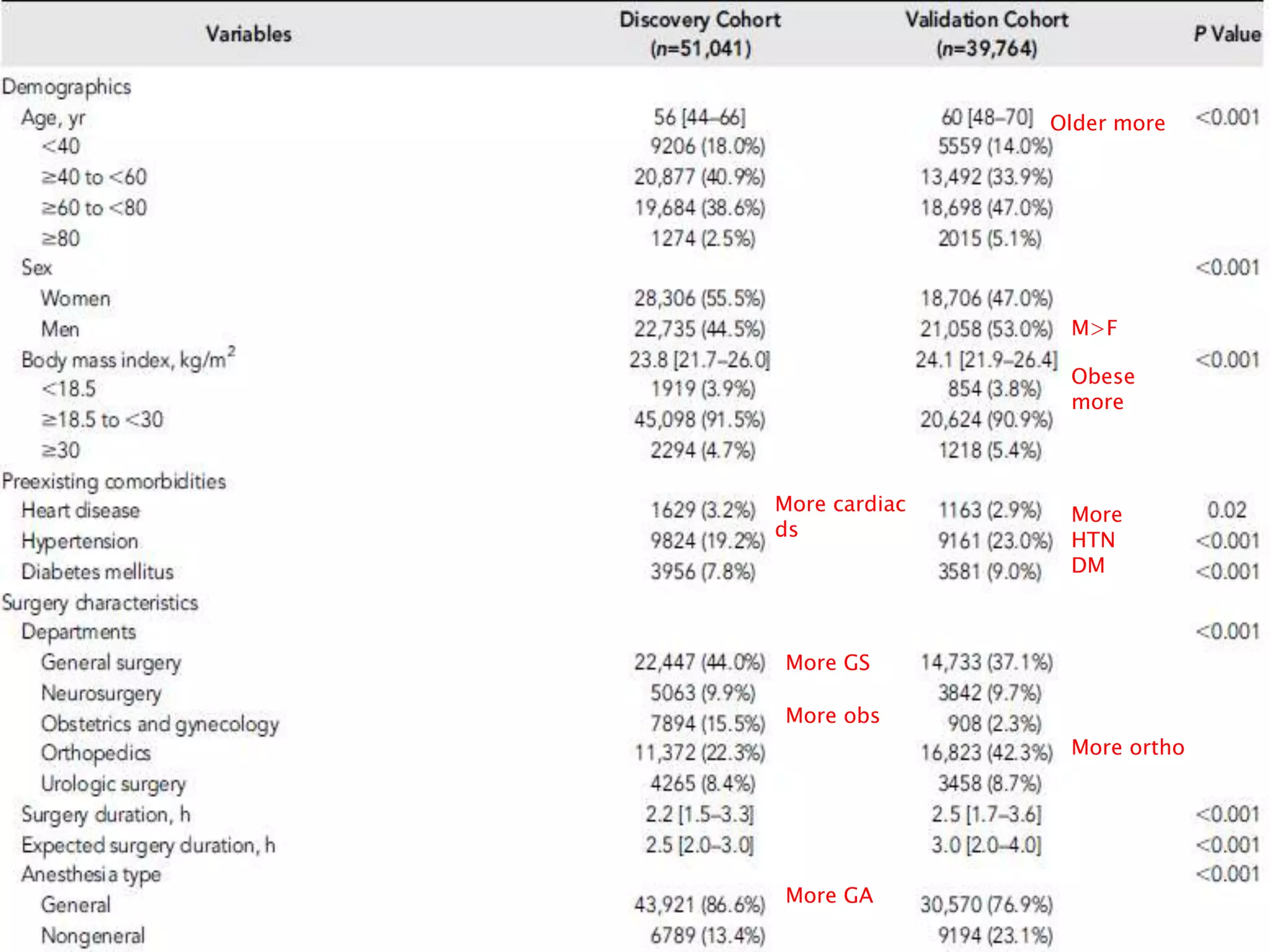
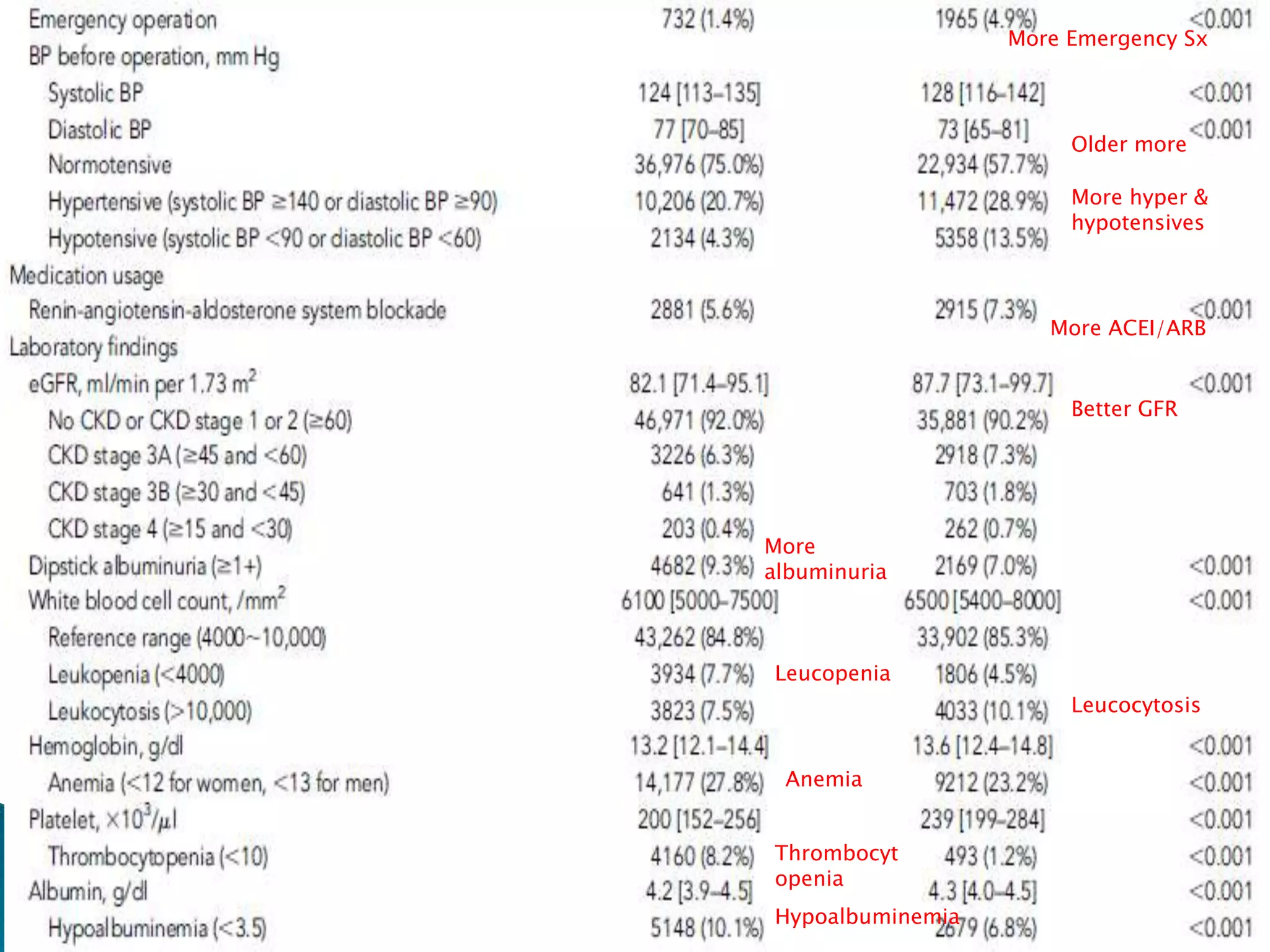
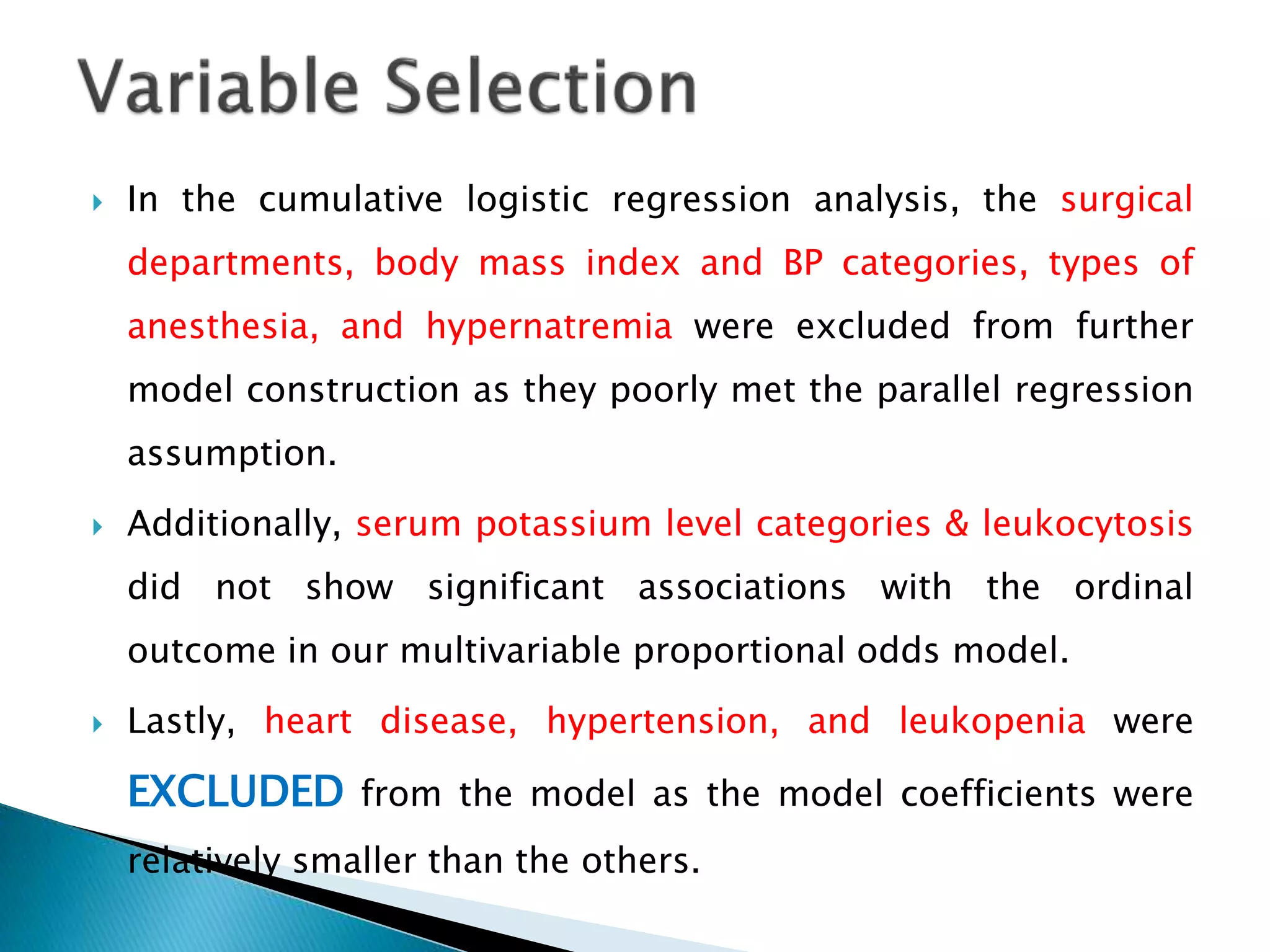
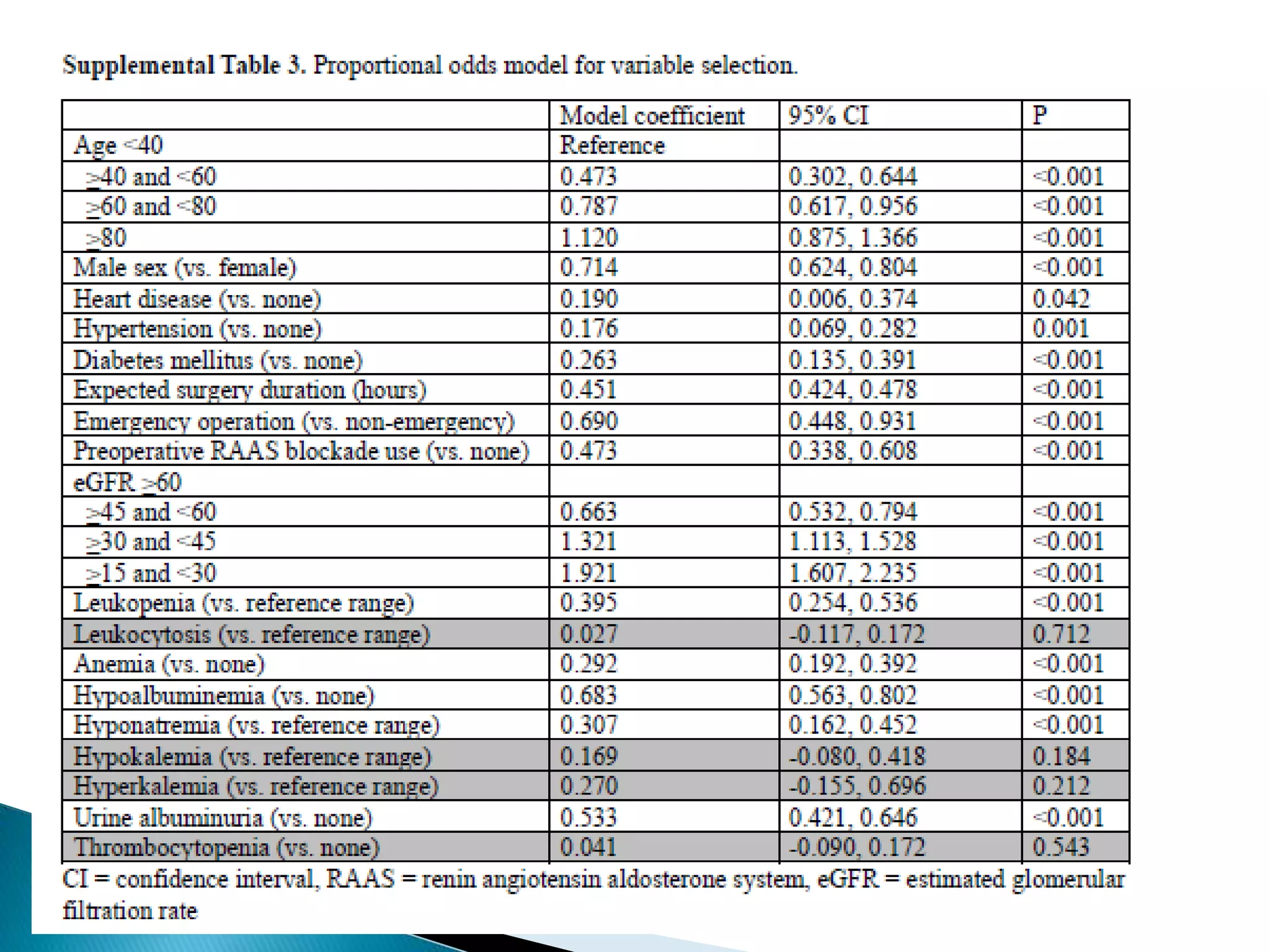
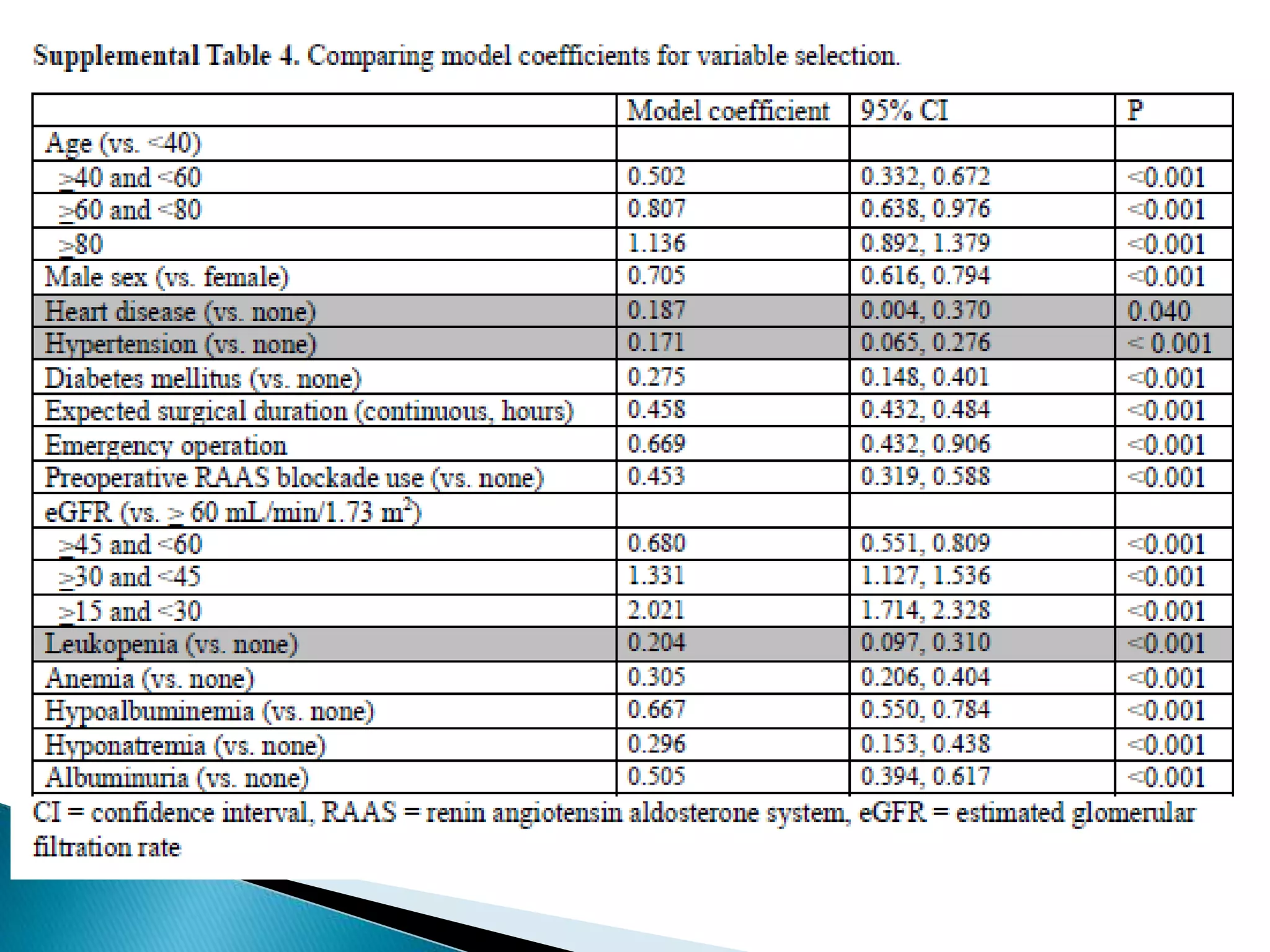
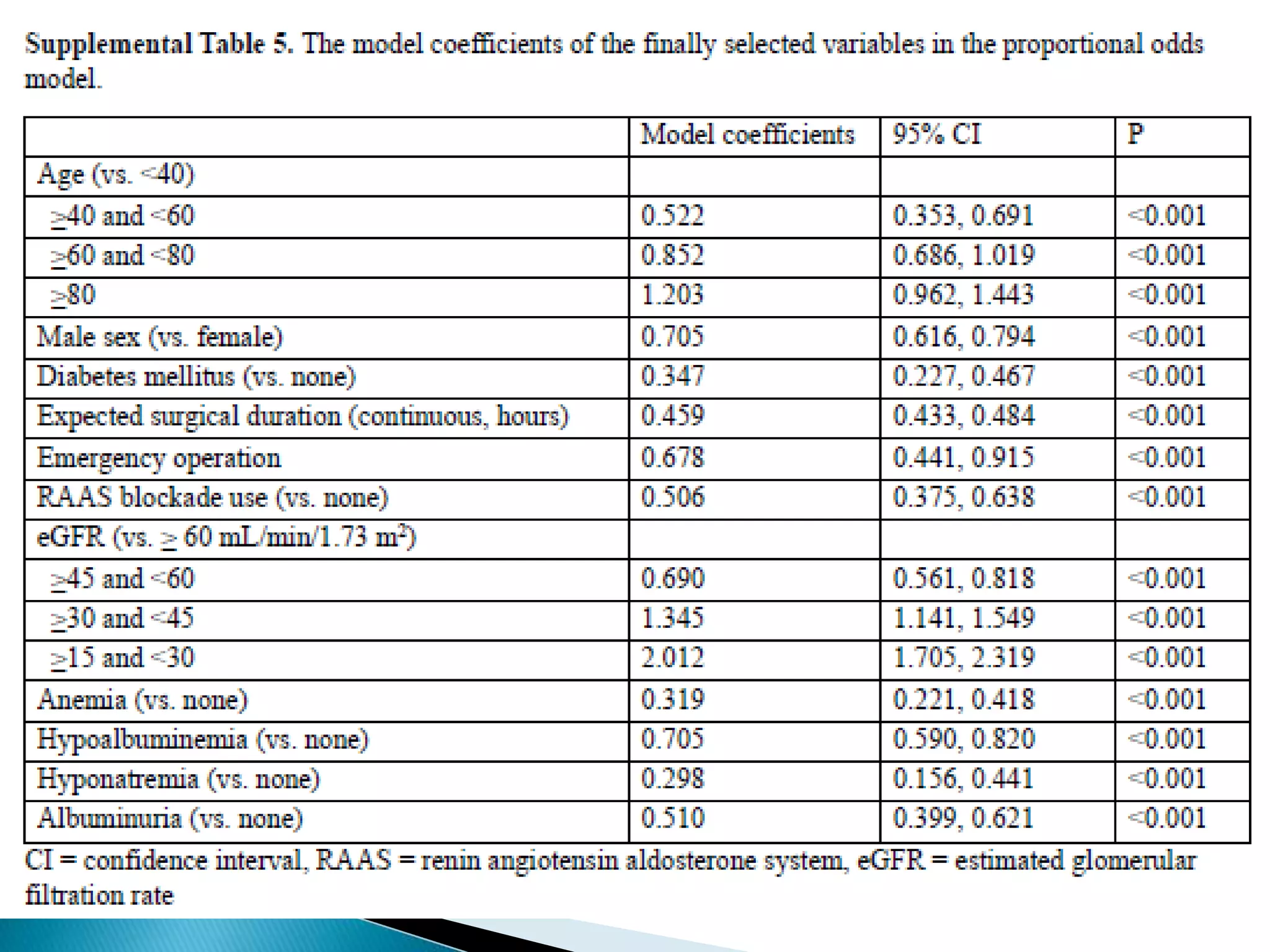
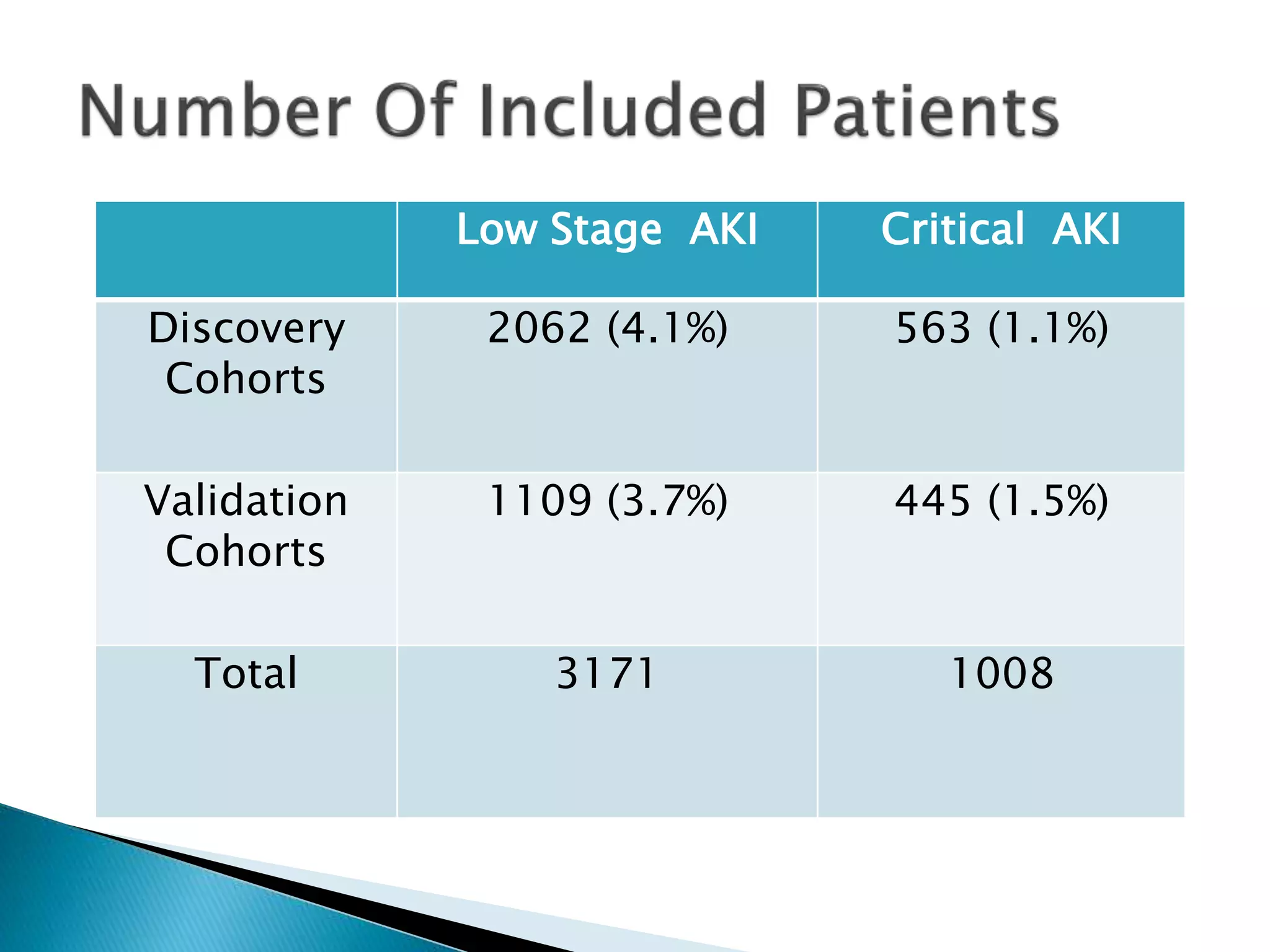
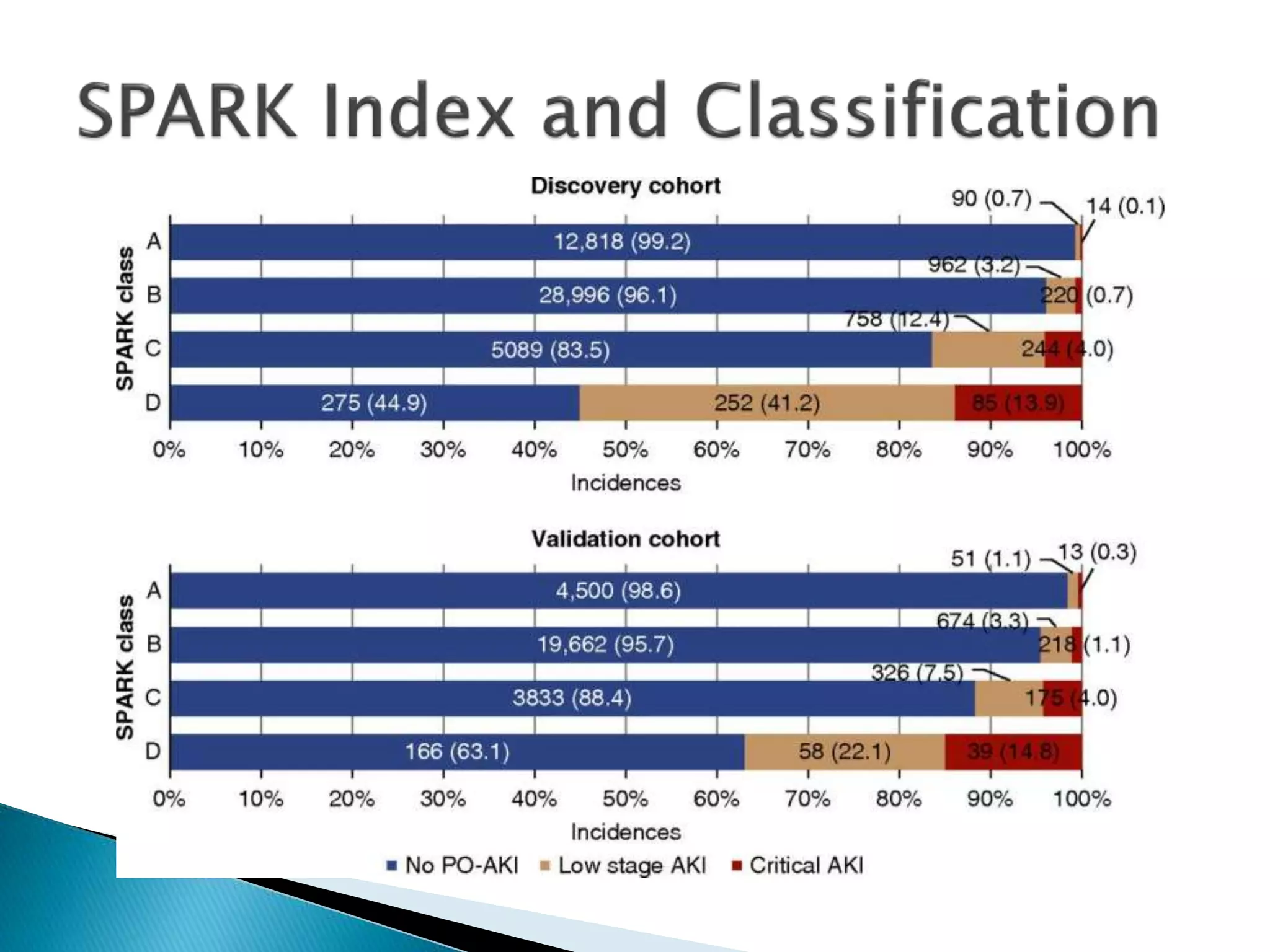
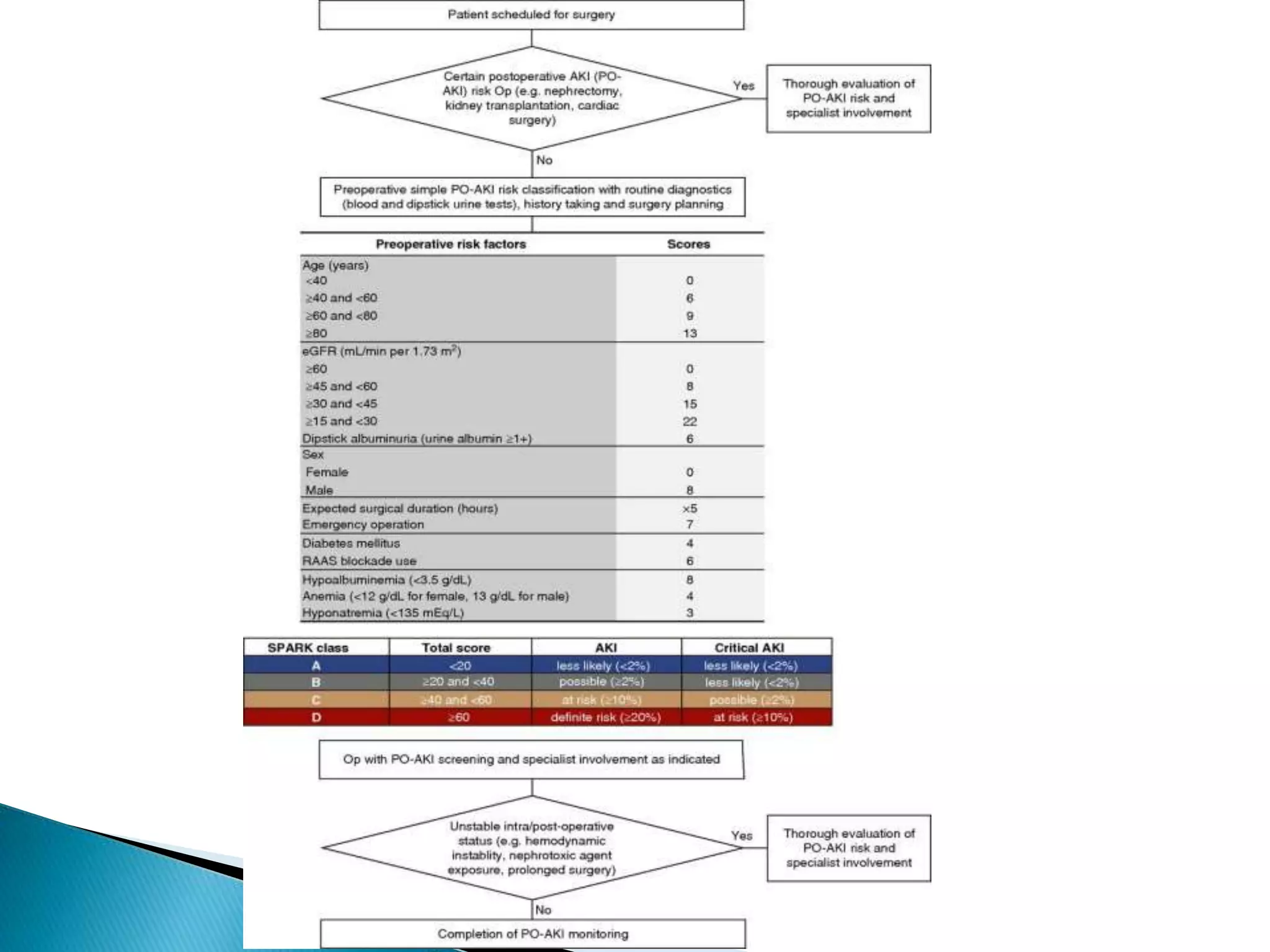
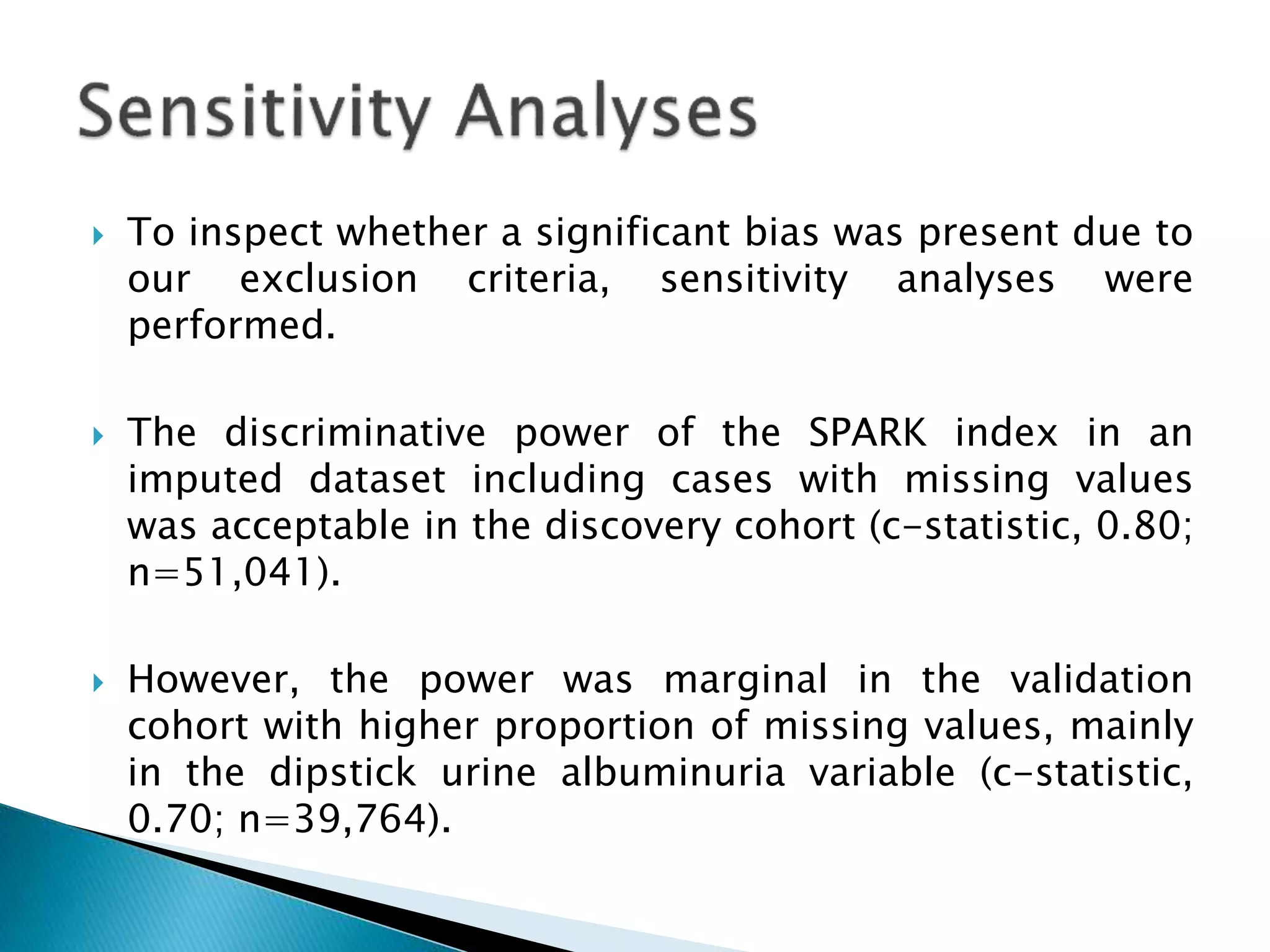
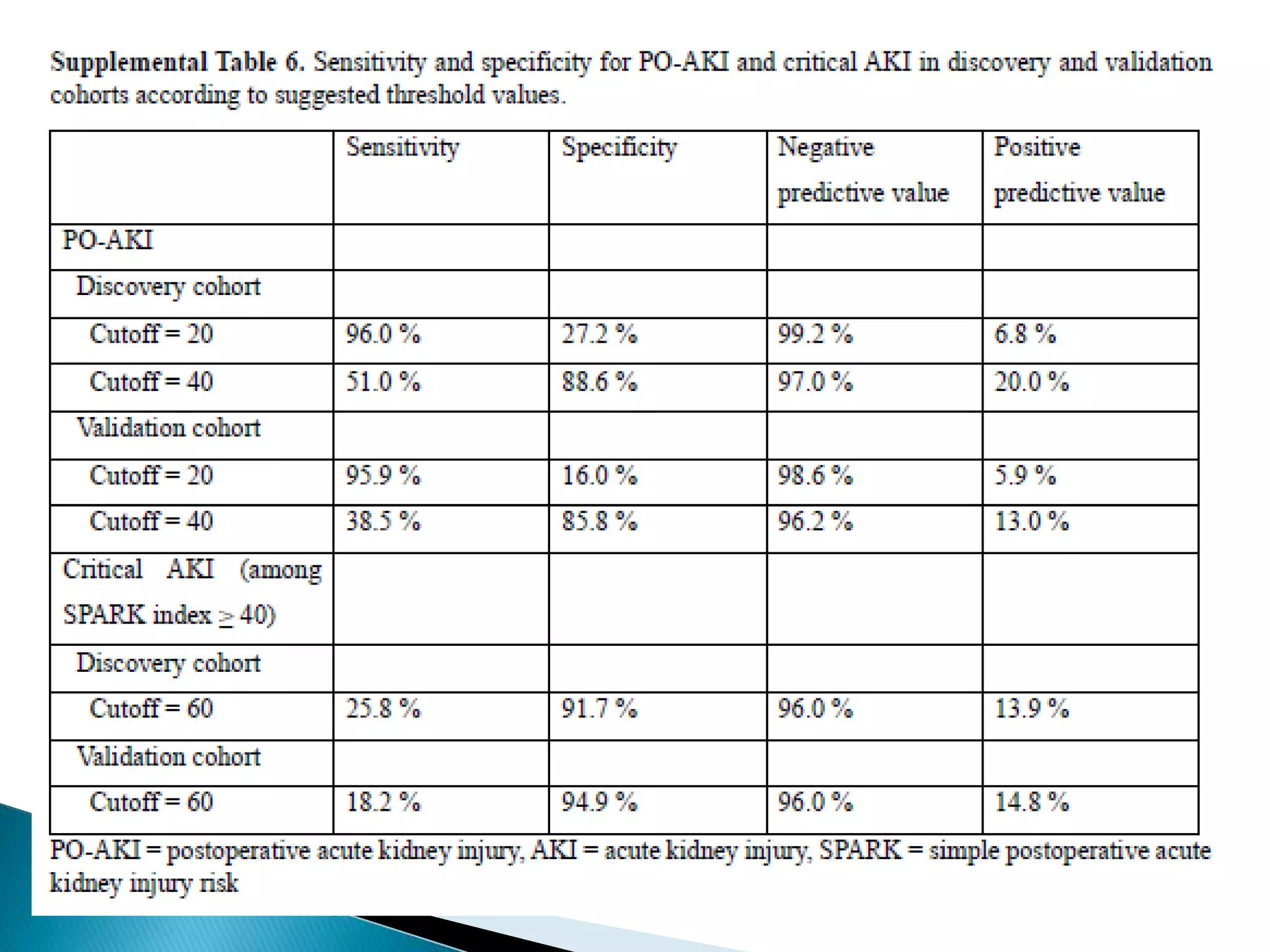
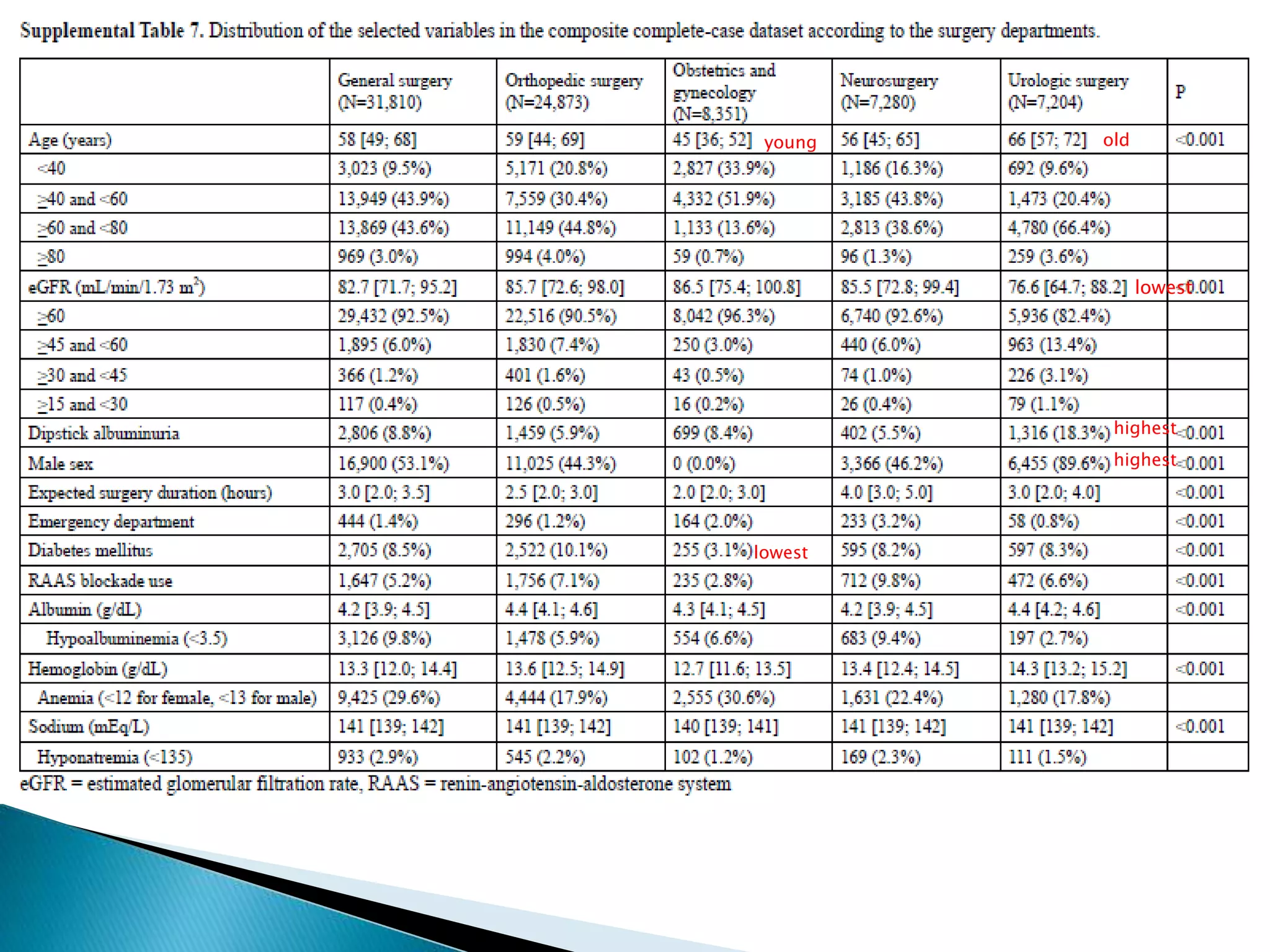
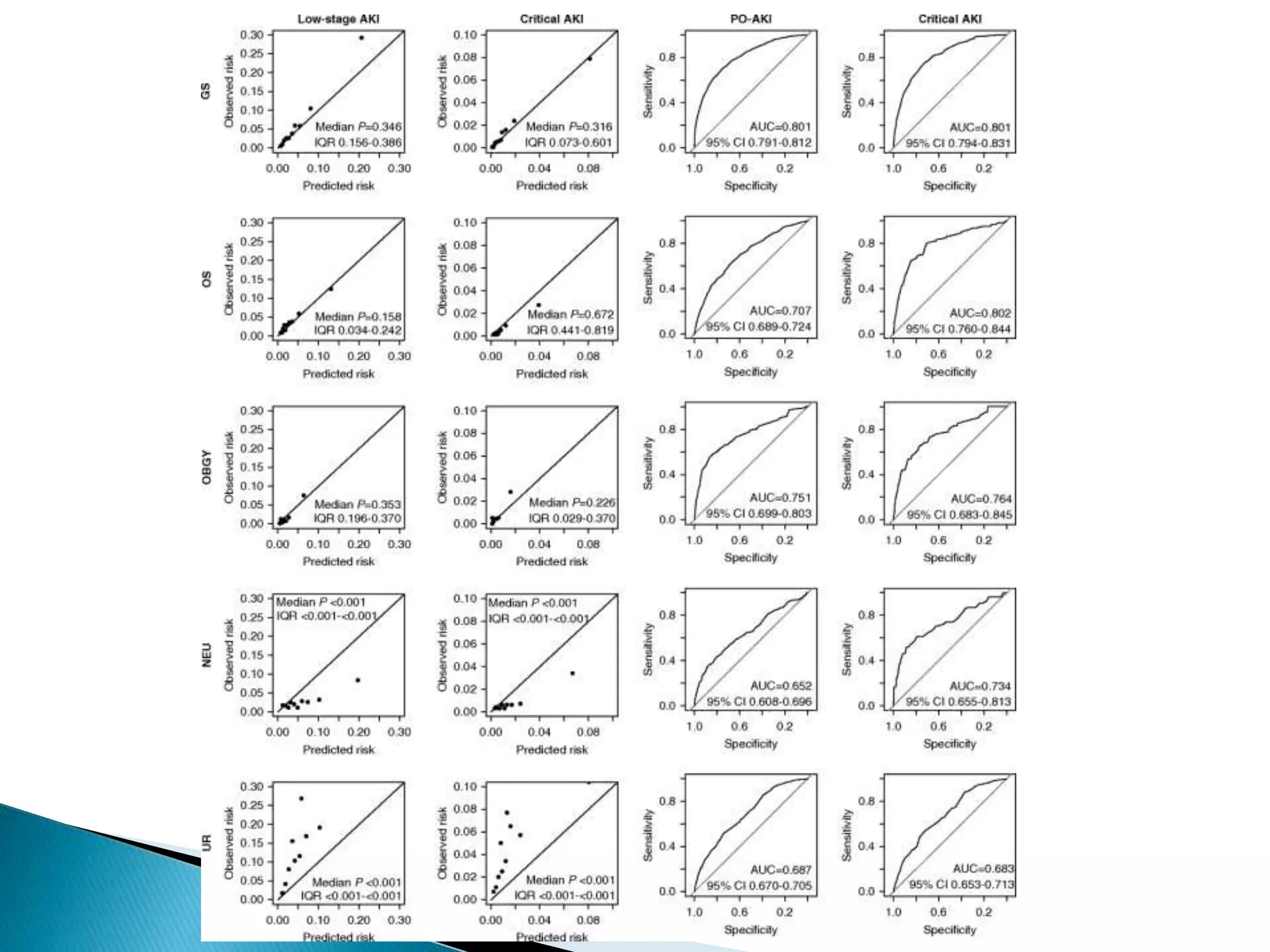
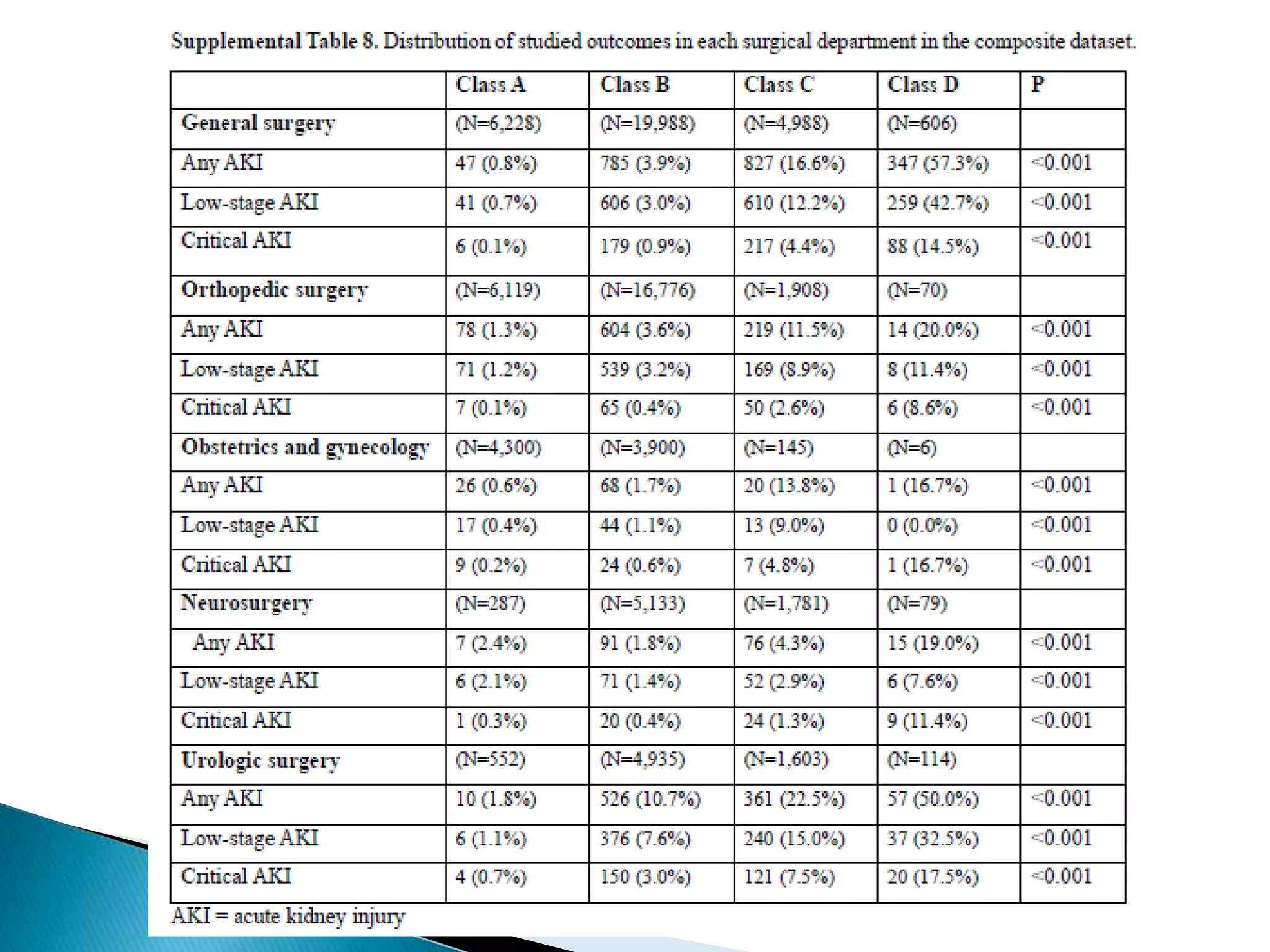
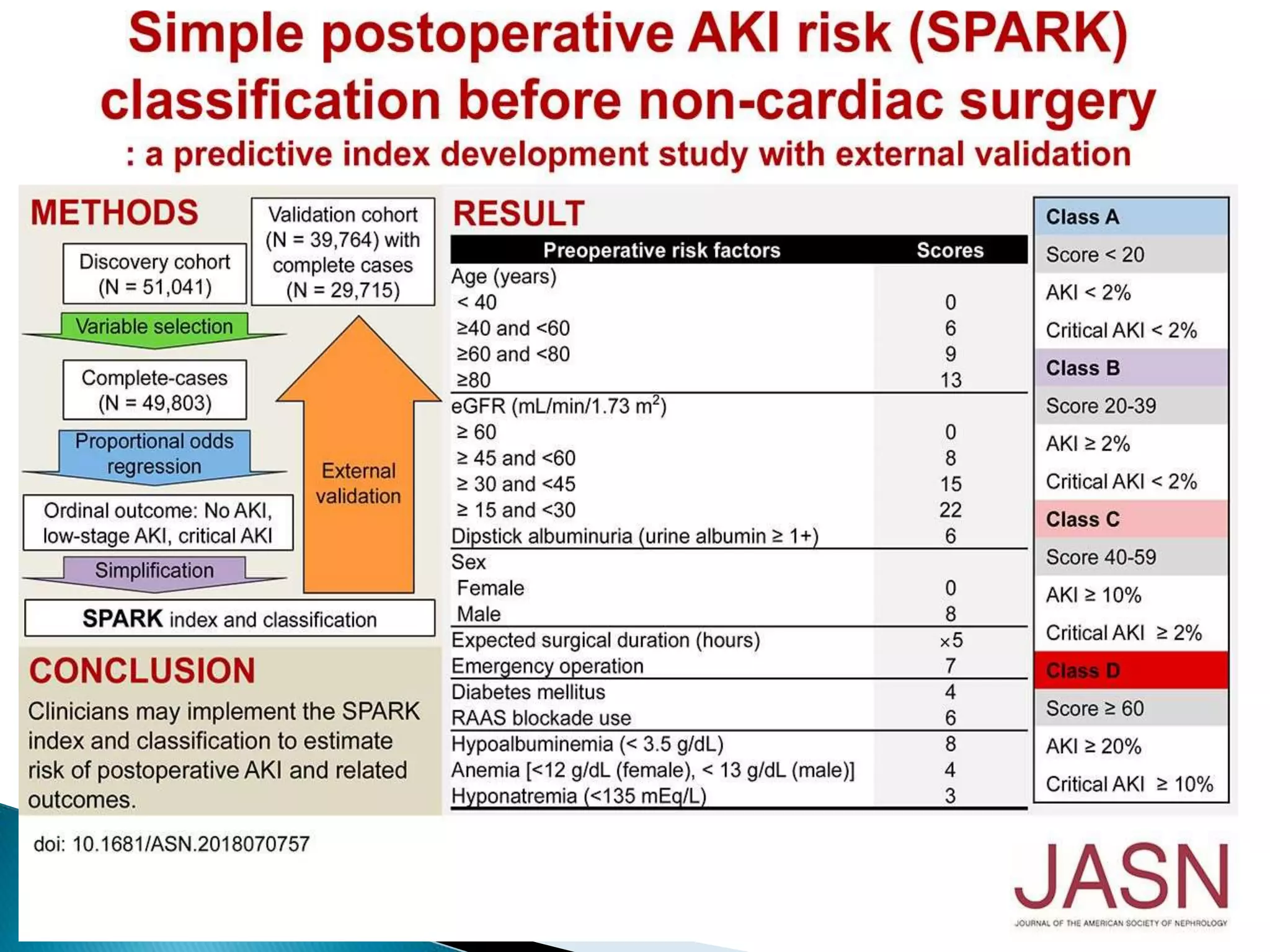
This study developed and validated a preoperative acute kidney injury (PO-AKI) risk prediction index called SPARK for noncardiac surgeries. Using data from two Korean hospitals, the study identified preoperative risk factors to stratify patients into four risk classes (A to D). Class A patients had the lowest PO-AKI risk while class D the highest. The simple index uses only preoperative variables and can help clinicians decide which patients need PO-AKI monitoring after surgery. While not perfect, the SPARK index provides a practical tool to predict and prevent PO-AKI.