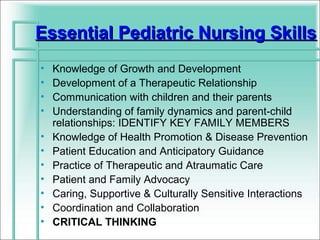
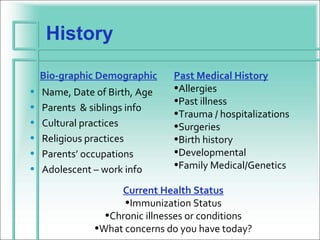
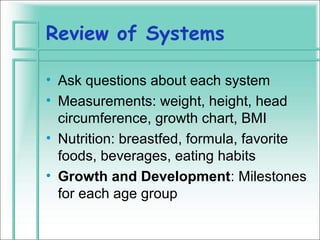
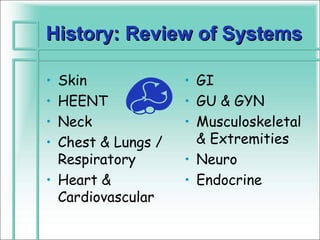
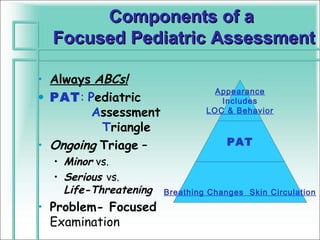
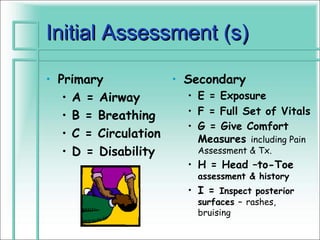
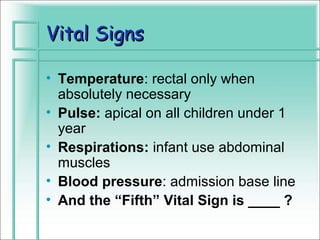
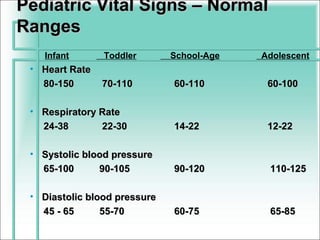
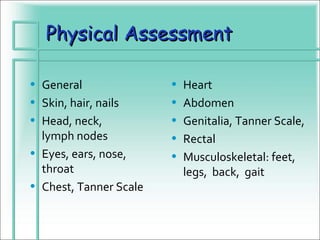
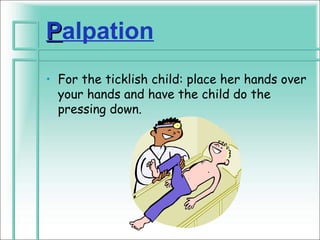
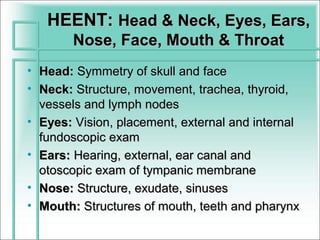
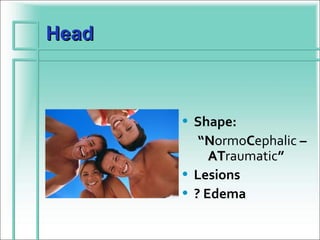
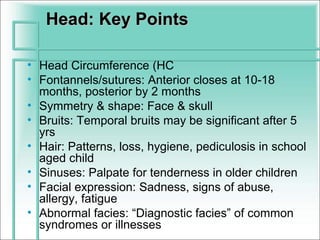
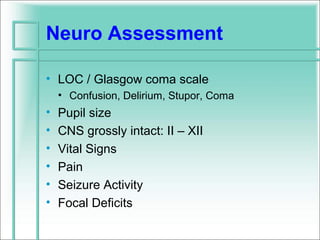
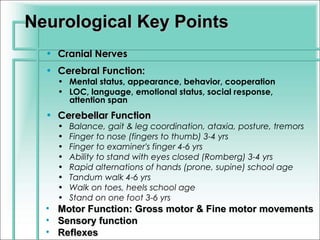
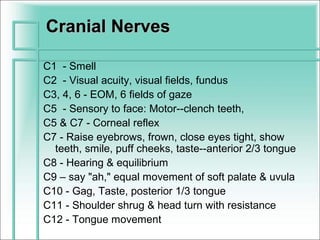
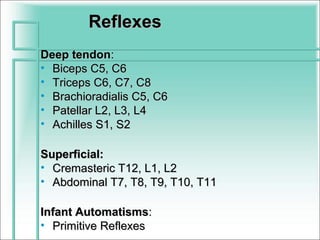
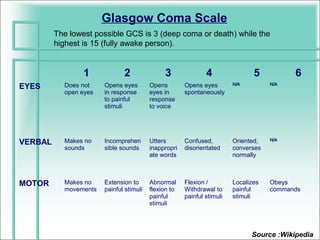
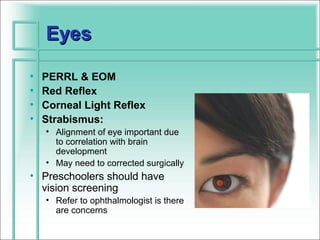
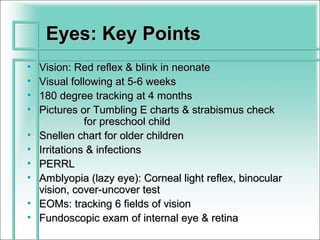
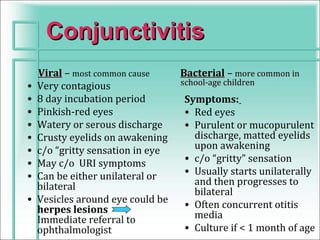
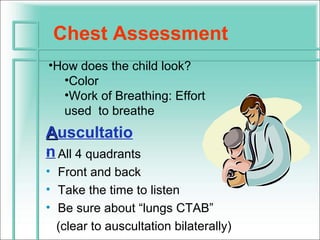
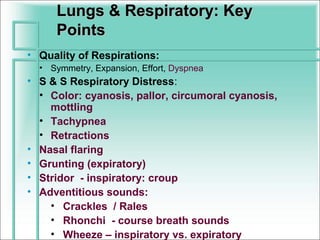
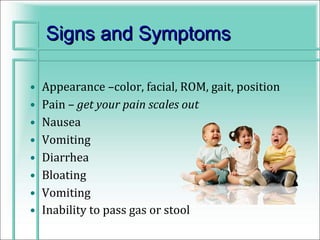
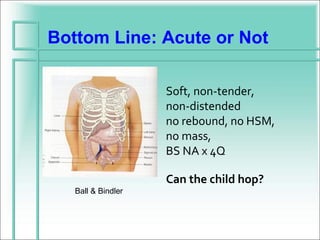
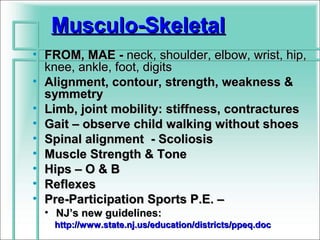
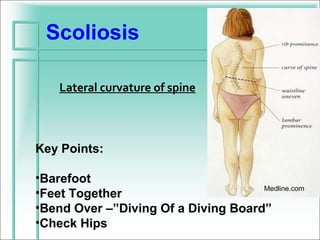
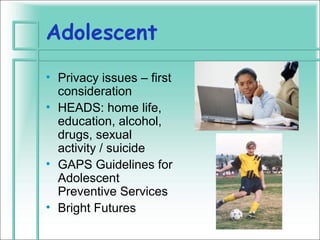
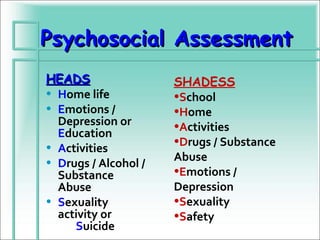
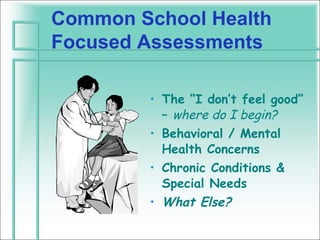
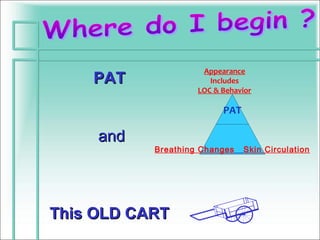
This document discusses the importance of assessment and triage in pediatric care. It outlines the essential components of a focused pediatric assessment, including evaluating the child's appearance, breathing, and skin circulation. The document also provides guidance on performing a thorough physical exam and neurological assessment of children.