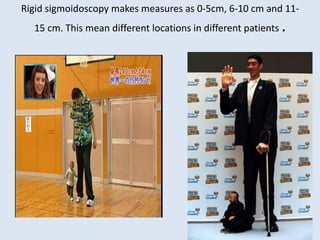
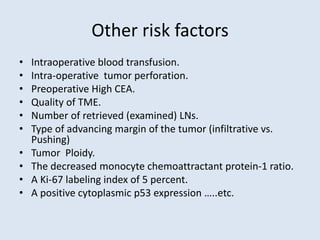
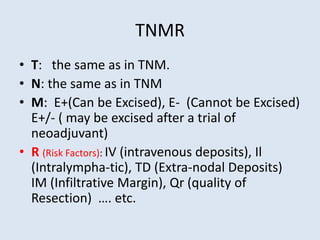
This document discusses the need for improved classification, staging, and grading of rectal cancer to enhance treatment planning and outcomes, questioning the adequacy of existing TNM classifications. It advocates for the use of MRI over rigid sigmoidoscopy for preoperative staging, proposing a modified TNMR system that incorporates additional risk factors affecting prognosis. The TNMR classification aims to provide a more comprehensive understanding of patient risk and to guide treatment strategies more effectively.