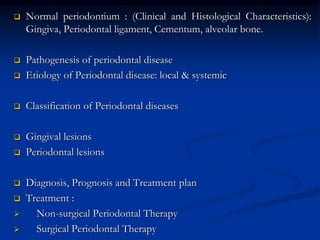
The document provides an overview of the normal anatomy of the periodontium. It describes the four main components - gingiva, periodontal ligament, cementum, and alveolar bone. It then discusses the histology and clinical characteristics of each component, with a focus on the gingiva. Key points include that the gingiva is made up of epithelium and connective tissue, with the epithelium consisting of sulcular, junctional, and oral epithelium. The connective tissue contains collagen fibers and cells. Clinically, healthy gingiva is pale pink, resilient, and has a stippling surface texture.