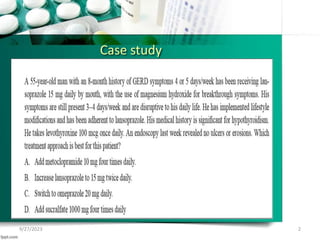
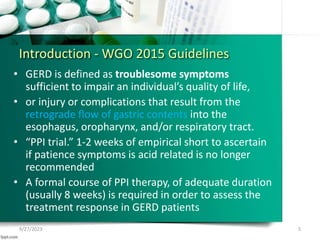
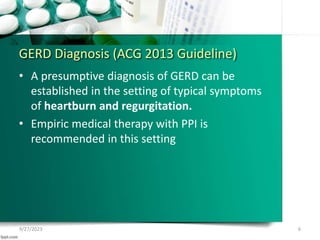
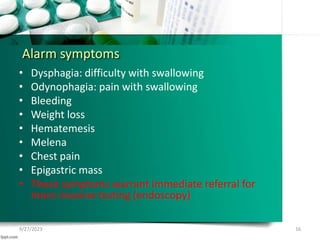
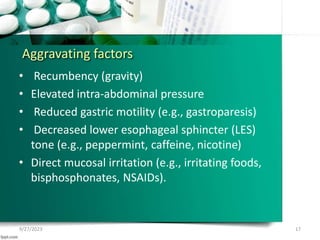
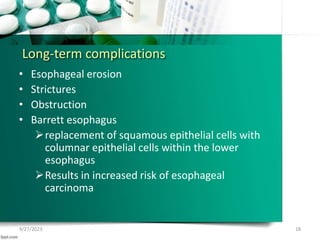
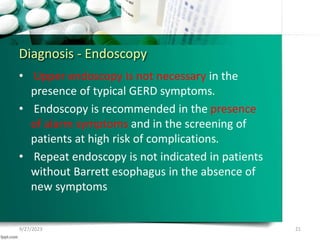
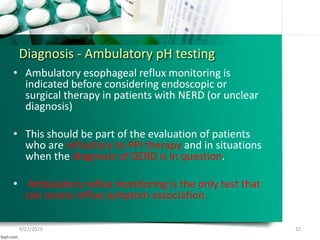
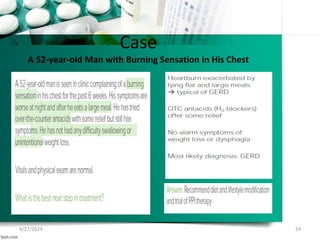
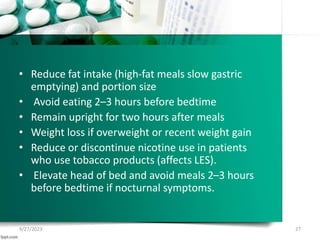
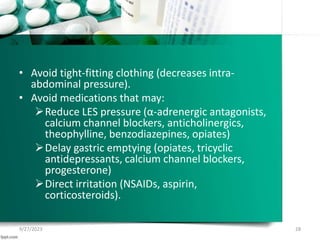
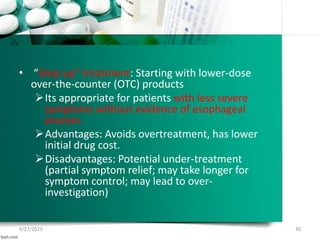
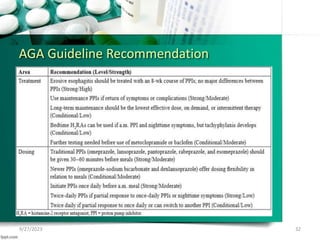
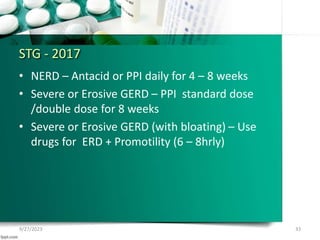
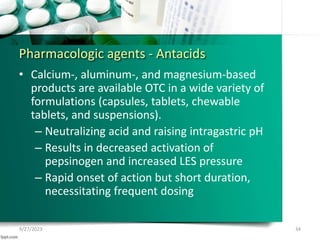
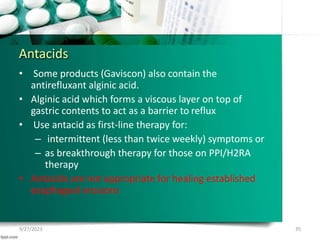
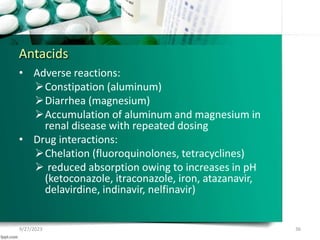
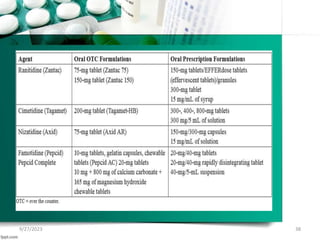
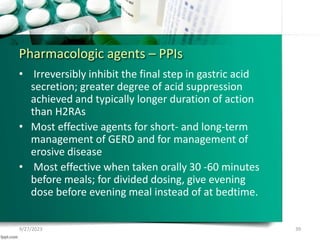
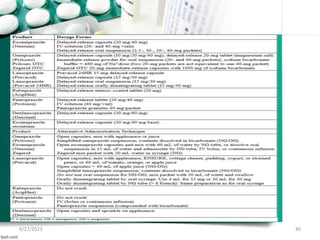
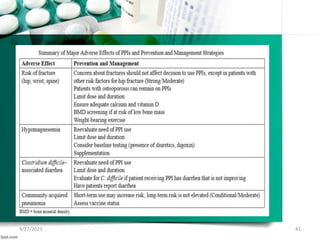
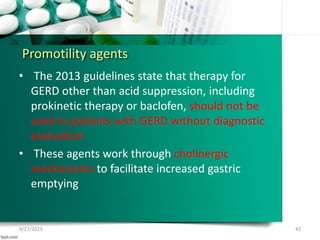
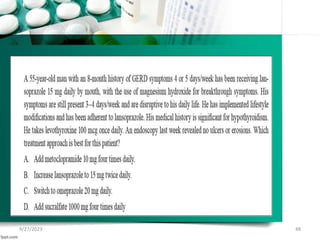
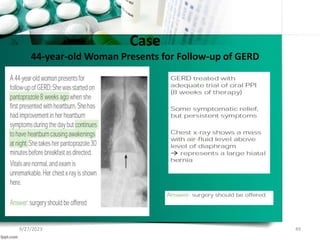
This document provides an overview of gastroesophageal reflux disease (GERD), including its pathophysiology, symptoms, complications, diagnosis, and treatment strategies. It defines GERD and distinguishes between NERD and ERD. Diagnosis is based on symptoms, though endoscopy may be used for alarm symptoms or treatment failure. Treatment involves lifestyle changes, antacids, H2 blockers, proton pump inhibitors, and sometimes promotility or surgical options. The goal of treatment is symptom relief and prevention of complications like Barrett's esophagus.